In this issue:
- Key players in the private health insurance marketplace
- Emerging issues in private health insurance
- Key facts about arthritis and private health insurance
- Adherence
- What is the role of insurance companies/advisors?
- Impact of Arthritis in the Workplace
- What can employers do for employees living with arthritis?
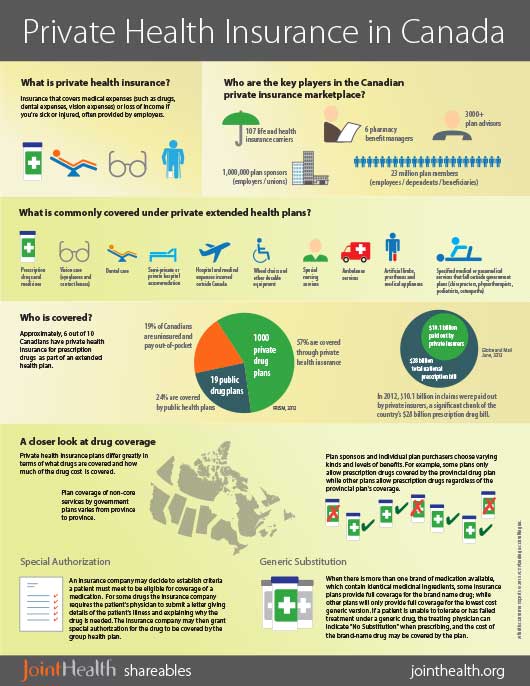
Arthritis Consumer Experts members are taking a growing interest in the private health insurance market. More than 23 million Canadians depend on private insurance to cover their prescription medication costs.
The high prevalence of arthritis and impact of certain types, such as osteoarthritis, rheumatoid arthritis, and ankylosing spondylitis, are placing increasing pressure on plan sponsors (employers/unions) faced with dramatically growing number of arthritis medication claims and risks associated with absence and disability costs.
Key players in the private health insurance marketplace
| Insurer An insurance company that issues policies and promises to pay benefits. |
|
| Pharmacy Benefit Manager A provider of services, including claims processing, home delivery services, and benefit-design consultation (e.g. prescription drug coverage) for insurance carriers, third-party benefits administrators, the public sector and other organizations that provide health benefits. |
|
| Plan sponsor The holder of a group insurance, group benefit policy, group pension, or group savings plan. It can be any organization that provides group benefits to its members (e.g. an employer, union or association). |
|
| Plan member The person insured under a group insurance, group benefit policy, group pension, or group savings plan (e.g. an employee, union member or association member). |
|
| Plan advisor A person who is licensed by a provincial or territorial regulator to sell life insurance, accident and sickness insurance, group insurance and segregated funds. Also called an agent or a broker. |
Emerging issues in private health insurance
ACE members have identified increased reporting of issues involving insurers and coverage of arthritis treatments, including:
| Case management of drug claims: Insurer reviews physician's proposed treatment plan to ensure it's "reasonable"; identifies alternative treatments; monitors adherence; limits payment. | |
| Preferred pharmacy networks: "Requiring" consumers to purchase from specific pharmacies. | |
| Therapeutic substitution: Private plan recommends/requires that patient uses a different drug than the one prescribed. | |
| Tiered formulary: Some plans require patient to use a cheaper drug than the one prescribed through tiered formulary where the patient will have to pay a higher percent co-pay for selected drugs. | |
| Special authorization: Most major insurers have a special authorization process for selected drugs, including biologic treatments, which might delay the access to optimal treatment for a specific patient. |
Key facts about arthritis and private health insurance
- One in six Canadians has some form of arthritis. Close to three in five people (58%) with arthritis are under 65 years of age, which has significant impact on participation in the labour force.
- One out of every 136 Canadian workers lives with rheumatoid arthritis; that will increase to one in 68 workers by 2020.
- The cost of biologic response modifiers to treat forms of inflammatory arthritis is now one of the fastest growing categories of medications for employer sponsored private plans across Canada.
- Early referral for diseases such as rheumatoid arthritis and ankylosing spondylitis can lead to early diagnosis and treatment with better long-term results helping to decrease pain and swelling, maintain joint structure and function and prevent permanent disability and loss of employment.
- Studies by Arthritis Research Canada and other leading researchers have found that early treatment with medications can reduce the short and long-term costs associated with arthritis, work disability claims being largest among them. Quite often, appropriate arthritis medication or treatment can mean the difference between lifelong disability and return to a mostly normal life.
- The ability for plan members living with arthritis to have meaningful conversations about their unique health challenges with their healthcare professional – from family physician pharmacist to occupational- and physio-therapists – is vitally important to address absenteeism and presenteeism focused on medication management.
Adherence
| Whether it is voluntary or involuntary and whether it is not filling a prescription to begin with, skipping doses, missing refills, or discontinuing medications altogether, patients not taking medications properly is an everyday occurrence. This is problematic when considering the negative outcomes of not taking medications properly, which include unnecessary worsening of symptoms or progression of the condition, increased health care visits, need for more medications, hospitalizations, and even death. |
Adherence by the numbers: 50% the proportion of patients with chronic disease who are non-adherent to medications. 69% the proportion of medication-related hospitalizations due to non-adherence. $7-9 billion estimated annual cost of nonadherence in Canada (in 1995). |
What is the role of insurance companies/advisors?
| Private health insurance companies have the potential to be leaders in Canada promoting prevention and patient-focused treatment and care of arthritis. | |
| With a comprehensive understanding of arthritis in the workplace, insurance companies and advisors can provide plans with fair access to medication that ensures the plan member receives the care needed to maintain productivity, while reducing overall absenteeism and presenteeism in the workplace. |
Impact of Arthritis in the Workplace
Arthritis is the most common cause of work disability in Canada, resulting in both poor quality of life and workplace limitations.
Of particular relevance for insurers is the category of inflammatory arthritis (rheumatoid arthritis, ankylosing spondylitis, psoriatic arthritis and gout), which affects approximately 2.8% of Canadians.
Rheumatoid arthritis (RA) strikes more than 272,000 people, approximately 1% of the Canadian adult population, which will increase to 1.3% over the next 30 years. Approximately 0.74% of the employed labour force, or 1 in 136 workers is suffering from RA. Within a generation, this will increase to 1.5%, or 1 in 68 workers. Within ten years of disease onset, up to 50% of people living with rheumatoid arthritis are work disabled if untreated or undertreated.
Other forms of arthritis affect about 4.6 million (approximately one out of every six) Canadians, which is expected to increase by nearly 50% in the next decade. There are currently more than 4.4 million people living with osteoarthritis.
"49%
of Canadians living with arthritis have not told their employer. As a result, these employers and employees are unable to work together to develop positive plans and approaches that make sense for both of them."
Within a generation (in 30 years), more than 10 million (or one in four) Canadians are expected to have osteoarthritis (OA). There will be a new diagnosis of osteoarthritis every 60 seconds, resulting in almost 30% of the employed labour force (one in three workers) having difficulty working due to OA. In addition, approximately 500,000 Canadians will be suffering with moderate to severe disability due to osteoarthritis.of Canadians living with arthritis have not told their employer. As a result, these employers and employees are unable to work together to develop positive plans and approaches that make sense for both of them."
While arthritis consumers are able to contribute mentally, their joints are in severe pain and they are likely to leave the workforce earlier than planned, including going on disability (18% within five years after diagnosis and 27% within 10 years after diagnosis). However, employers can work with their employees to create a workplace more conducive to people who have arthritis.
What can employers do for employees living with arthritis?

|
|
JointHealth™ shareables
"Whether it is with an infographic, video, or text, ACE looks for new ways to share healthcare information, research and policy in a way that is interesting and easy to understand. Our new program, JointHealth™ shareables, presents important health issues in one easy-to-navigate page."

