In this issue
- Getting "Patient Satisfaction" from Arthritis Health Care
- Who Answered the Surveys?
- The mind and emotional connection to the body
- The arthritis treatment experience
- Taking charge of what you can control
- Self-care at home
- Sharing your self-care success with your healthcare team
JointHealth™ insight Published January 2018

Getting “Patient Satisfaction” from
Arthritis Health Care What You Told ACE
In Fall 2017, Arthritis Consumer Experts (ACE) surveyed you to tell us about your own experiences with arthritis health care, what you ideally expect from the health care system, and about your own arthritis experiences.
Why? Because your views are invaluable for setting the direction of future health care planning, as well as identifying measurements to gauge whether the health care system is delivering what you want and need as arthritis patients.
In this issue of JointHealth™ insight, we share survey results and offer information to help you get more satisfaction from the health care system and improve your personal experience with arthritis.
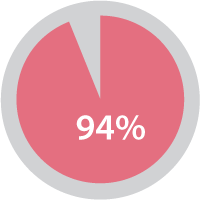
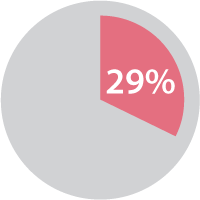
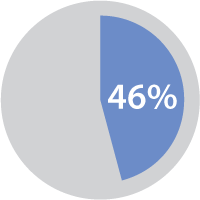
An important theme highlighted in the survey findings – one that has received a lot of research and media attention over the years but not necessarily in arthritis – is the psycho-emotional issues affecting people living with arthritis. Most respondents (94%) reported talking with their healthcare professional about pain or fatigue, but a significantly lower number said they were comfortable talking about depression (29%) and intimacy (6%), things previous research tells us greatly affect people with arthritis.
In fact, depression is considered a “comorbidity” of inflammatory types of arthritis (IA) such as rheumatoid arthritis (RA), ankylosing spondylitis (AS) and psoriatic arthritis (PsA). Ask anyone living with one of these diseases and they will tell you that it can be hard to maintain a sunny outlook on life when in debilitating pain and fatigue, and having to parse out energy in small amounts to get through their days at home and at work. Not only does depression make it that much harder to cope with the physical impact of arthritis, it can even make disease symptoms worse.
Based on the results of one of the international surveys, #RAMatters, which explored the outcomes and quality of life related areas most important to patients living with RA but are rarely researched or written about, ACE asked its members how they approach speaking about their arthritis. ACE members described the experience that from an outsider’s perspective (e.g. friend or work colleague), they didn’t look any different or show obvious physical signs of the pain and fatigue they were feeling inside. Respondents spoke about how people don’t understand types of inflammatory arthritis as well as other more common chronic diseases such as heart disease or breast cancer, so they had to first educate them what IA is and compare it to other autoimmune diseases like type 1 diabetes.
Most people can relate to those more common diseases and know how serious they are and get a better sense of what ACE members are going through. Some of you spoke about how horrible it is experiencing the stigma of having a disease people don’t understand and the depression it caused. As one ACE member said: “When people hear RA, they tend to think of their grandmother’s twisted-up hands. I tell them it’s more like cancer and my inflammation is my tumor. That gets their attention.”
Fortunately, inflammatory arthritis and depression are both treatable and it starts with patients understanding how to set treatment goals and practice positive self-care strategies.
The arthritis treatment experience
written (or electronic) document you create. Think of it like a “contract” to get better. For many people with arthritis this document “lives” with them throughout a life-long journey given no single form of arthritis is yet curable.
A majority (59%) of ACE survey respondents reported including clearly stated goals in their treatment plan, such as “I love to walk; I want to get back to walking around my neighbourhood so that in 6 months I can go on a walking vacation with my family.” However, less than half of respondents had prepared a list of steps to take to reach their treatment plan goals.

For those of you not using motivational steps, ACE recommends, for example, creating a “walking journal” to track your progress, and make a list of things to be mindful of that prevent you from reaching your goals, such as highlighting the need to protect the time and days you have chosen to do your walks.
Interestingly, few respondents noted motivational rewards as part of their treatment plan, something that can be quite helpful to “sticking with” the plan. Everyone likes to be rewarded for their efforts and accomplishments; it is human nature. We think the sweetest rewards come from oneself. For example, if you are a walker and you are half way to your walking distance goal to prepare for your family holiday, see if your finances will allow for a new pair of walking shoes, or a cheery new pair of socks designed for long distance walking. Even “toasting” your accomplishment at the family dinner table is a heart-warming gesture and motivational to continue working towards the larger goal.
Taking charge of what you can control
It is important for patients with IA not to blame themselves if a medication or non-medication treatment doesn’t work. There are many things about your disease that you can and cannot control, such as which joints the disease will affect, how severe your disease may be at time of diagnosis, whether you will have IA complications, among others.
However, you do control whether you follow the treatments as prescribed and other aspects of your treatment plan that you develop with your rheumatologist. Recognizing what things in your treatment plan and life that you have control over will give you focus and motivate you to follow through on the things you list in your plan. Patients with IA who “adhere” – or follow a treatment plan – do better short- and long-term.
Results from ACE’s mini surveys show that exercise is a vitally important part of respondents’ (54%) self-care plan.
When done safely, even high intensity exercise is good for patients with IA. The self-care aspects of your overall treatment plan might include things to improve your strength, mobility, and/or flexibility. Exercise is proved to help to improve your IA pain and overall well-being, even if you are currently experiencing pain and fatigue.
There are three general types of exercise you can consider including in your treatment plan:
Speaking to a dietician with knowledge about the dietary needs of people with IA is very helpful. Some dietician services are provided for free. Ask your rheumatologist’s office staff if they can recommend one. JointHealth.org is a good source for tips on dealing with sleep and fatigue issues, see the June 2007 issue of JointHealth™ insight for more information. Another excellent resource are the interviews contained in the #CRArthritis Facebook and Twitter Live event from the Canadian Rheumatology Association’s annual meeting. Highlights include presentations on exercise and the correlation of sex, smoking, and excess weight on arthritis
Other ACE survey respondents cited physiotherapy and occupational therapy as being extremely helpful. If your government or private health care plan don’t provide coverage for these services, ask your rheumatologist what types of things they might do for you, such as joint protection techniques, stretching or strengthening, that you might be able to safely do on your own.
Finally, ongoing disease education can help people with arthritis feel “on top of” their disease and helps to grow their “expertise” leading to greater empowerment and overall feeling of life control. Seeking out evidence-based web sites and resources materials is important to your life-long learning journey.
Self-care at home
Finally, respondents offered terrific insights in the open-ended survey questions. When asked what they regularly do to deal with the challenges and frustration of living with their arthritis, a number of great ideas were shared:
One of the most common responses from ACE members was the use of ice and heat, especially in the early days of your disease:
Sharing your self-care success with your healthcare team
You know your body best and what does – or does not – feel right for you. Trust what your body is telling you and do your best to share those things with your health care team. As mentioned earlier, keeping an arthritis journal is proved to help patients better manage the “details” of their disease, especially with their health care providers.
The aspects of your progress in between visits you need to share with your rheumatologist and other members of your healthcare team (and family and friends if you choose) include:
Listening to you
We hope you find this information of use. Please tell us what you think by writing to us or emailing us at feedback@jointhealth.org. Through your ongoing and active participation, ACE can make its work more relevant to all Canadians living with arthritis.
Update your email or postal address
Please let us know of any changes by contacting ACE at feedback@jointhealth.org. This will ensure that you continue to receive your free email or print copy of JointHealth™ insight.
Arthritis Consumer Experts (ACE)
Who We Are
Arthritis Consumer Experts (ACE) provides research-based education, advocacy training, advocacy leadership and information to Canadians with arthritis. We help empower people living with all forms of arthritis to take control of their disease and to take action in healthcare and research decision making. ACE activities are guided by its members and led by people with arthritis, leading medical professionals and the ACE Advisory Board. To learn more about ACE, visit: www.jointhealth.org
Acknowledgements
Over the past 12 months, ACE received grants-in-aid from: Amgen Canada, Arthritis Research Canada, AstraZeneca Canada, Canadian Biosimilars Forum, Canadian Institutes of Health Research, Celgene, Eli Lilly Canada, Hoffman-La Roche Canada Ltd., Merck Canada, Novartis, Pfizer Canada, Sandoz Canada, Sanofi Canada, St. Paul’s Hospital (Vancouver), UCB Canada, and the University of British Columbia.
ACE also receives unsolicited donations from its community members (people with arthritis) across Canada.
ACE thanks funders for their support to help the nearly 5 million Canadians living with osteoarthritis, rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis and the many other forms of the disease. ACE assures its members, academic and healthcare professional collaborators, government and the public that the work of ACE is free from influence of its funders.
Disclaimer
The material contained on this website is provided for general information only. This website should not be relied on to suggest a course of treatment for a particular individual or as a substitute for consultation with qualified health professionals who are familiar with your individual medical needs. Should you have any healthcare related questions, you should contact your physician. You should never disregard medical advice or delay in seeking it because of something you have read on this or any website.
This site may provide links to other Internet sites only for the convenience of World Wide Web users. ACE is not responsible for the availability or content of these external sites, nor does ACE endorse, warrant or guarantee the products, services or information described or offered at these other Internet sites.
Although the information presented on this website is believed to be accurate at the time it is posted, this website could include inaccuracies, typographical errors or out-of-date information. This website may be changed at any time without prior notice.

Getting “Patient Satisfaction” from
Arthritis Health Care What You Told ACE
Why? Because your views are invaluable for setting the direction of future health care planning, as well as identifying measurements to gauge whether the health care system is delivering what you want and need as arthritis patients.
In this issue of JointHealth™ insight, we share survey results and offer information to help you get more satisfaction from the health care system and improve your personal experience with arthritis.
Who answered the surveys?
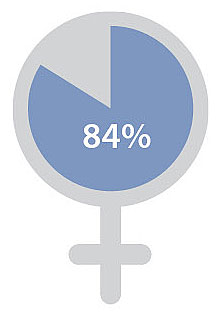
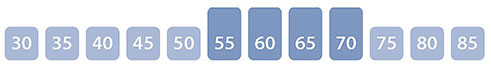
| 84% Women |
 |
| Majority of respondents had rheumatoid arthritis and osteoarthritis, followed by fibromyalgia and ankylosing spondylitis |
 |
| Ages range from 30 to 85, with the majority between 55-70 |
 |
| Majority of respondents from Ontario, British Columbia, Alberta, Saskatchewan and Nova Scotia |
 |
|
The mind and emotional connection to the body
|
An important theme highlighted in the survey findings – one that has received a lot of research and media attention over the years but not necessarily in arthritis – is the psycho-emotional issues affecting people living with arthritis. Most respondents (94%) reported talking with their healthcare professional about pain or fatigue, but a significantly lower number said they were comfortable talking about depression (29%) and intimacy (6%), things previous research tells us greatly affect people with arthritis.
 |
 |
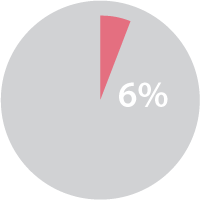 |
| Pain and fatigue | Depression | Intimacy |
| ACE survey respondents also highlighted how depression not only physically isolates them from family, friends and co-workers, but prevents them from sharing their feelings about the disease and its impact. Nearly 50% of respondents spoke about how difficult it was to talk about the pain and difficulties living with arthritis and asking for, and accepting, help. |
 Just talking difficulties |
Most people can relate to those more common diseases and know how serious they are and get a better sense of what ACE members are going through. Some of you spoke about how horrible it is experiencing the stigma of having a disease people don’t understand and the depression it caused. As one ACE member said: “When people hear RA, they tend to think of their grandmother’s twisted-up hands. I tell them it’s more like cancer and my inflammation is my tumor. That gets their attention.”
Fortunately, inflammatory arthritis and depression are both treatable and it starts with patients understanding how to set treatment goals and practice positive self-care strategies.
|
“When people hear RA, they tend to think of their grandmother’s twisted-up hands. I tell them it’s more like cancer and my inflammation is my tumor. That gets their attention.”
|
The arthritis treatment experience
|
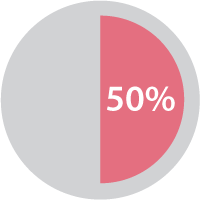
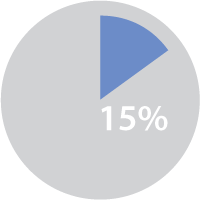
What ACE survey respondents told us about their current experience of arthritis treatment is important. A high number (70%) of respondents discussed their treatment goals and preferences for therapy with a health professional, including 59% expressing their dissatisfaction with their current treatment. While we don’t know what aspects of their treatment they were dissatisfied with, it is encouraging that respondents were discussing these things during the clinical visit. When treatment goals are discussed, the pros and cons of either current or future treatments are evaluated, and shared decision-making between health professional and patient occurs, patients get closer to “working their plan” and getting satisfaction from it overall. So that’s the theory, but what does it look like in practice? A treatment goal can be as simple as a statement like “I want my treatment/treatment plan to address my pain”, or, “I want to get back to full-time work”. These are real and tangible goals for both you and your health professional. A treatment plan clearly outlines the things you and your healthcare provider will do together to help you (and them) achieve your goals and best manage your RA. It is usually a |
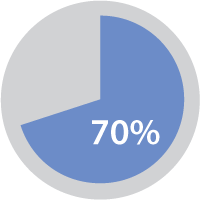 Discussed  Dissatisfied  Clearly state |
A majority (59%) of ACE survey respondents reported including clearly stated goals in their treatment plan, such as “I love to walk; I want to get back to walking around my neighbourhood so that in 6 months I can go on a walking vacation with my family.” However, less than half of respondents had prepared a list of steps to take to reach their treatment plan goals.

|
Setting treatment goals is one of the most important things you and your family doctor or rheumatologist will do in your life with arthritis.
|
For those of you not using motivational steps, ACE recommends, for example, creating a “walking journal” to track your progress, and make a list of things to be mindful of that prevent you from reaching your goals, such as highlighting the need to protect the time and days you have chosen to do your walks.
Interestingly, few respondents noted motivational rewards as part of their treatment plan, something that can be quite helpful to “sticking with” the plan. Everyone likes to be rewarded for their efforts and accomplishments; it is human nature. We think the sweetest rewards come from oneself. For example, if you are a walker and you are half way to your walking distance goal to prepare for your family holiday, see if your finances will allow for a new pair of walking shoes, or a cheery new pair of socks designed for long distance walking. Even “toasting” your accomplishment at the family dinner table is a heart-warming gesture and motivational to continue working towards the larger goal.
ACE has great information to help you create a treatment plan in the "Disease Spotlight" page of our website.
Taking charge of what you can control
It is important for patients with IA not to blame themselves if a medication or non-medication treatment doesn’t work. There are many things about your disease that you can and cannot control, such as which joints the disease will affect, how severe your disease may be at time of diagnosis, whether you will have IA complications, among others.
However, you do control whether you follow the treatments as prescribed and other aspects of your treatment plan that you develop with your rheumatologist. Recognizing what things in your treatment plan and life that you have control over will give you focus and motivate you to follow through on the things you list in your plan. Patients with IA who “adhere” – or follow a treatment plan – do better short- and long-term.
Results from ACE’s mini surveys show that exercise is a vitally important part of respondents’ (54%) self-care plan.
When done safely, even high intensity exercise is good for patients with IA. The self-care aspects of your overall treatment plan might include things to improve your strength, mobility, and/or flexibility. Exercise is proved to help to improve your IA pain and overall well-being, even if you are currently experiencing pain and fatigue.
There are three general types of exercise you can consider including in your treatment plan:
- Range-of-motion exercises: Joints are moved through as full range of motion as possible, to help patients from losing mobility in affected joints;
- Strengthening exercises: These help patients gain muscle mass and increase muscle strength. Strong muscles can help to protect joints; and
- Aerobic exercises: These help patients improve heart and lung function, improve strength and reduce inflammation and pain, and help with self-esteem and self-confidence.
 |
 |
 |
 |
| Exercise | Diet | Sleep | Smoking |
Other ACE survey respondents cited physiotherapy and occupational therapy as being extremely helpful. If your government or private health care plan don’t provide coverage for these services, ask your rheumatologist what types of things they might do for you, such as joint protection techniques, stretching or strengthening, that you might be able to safely do on your own.
 |
 |
 |
| Ongoing disease education |
Developing and following healthy life style practices |
Health Journaling |
 |
 |
| Self-directed, at home treatments |
Prescription excercise, physical activity and sport for pleasure |
Self-care at home
Finally, respondents offered terrific insights in the open-ended survey questions. When asked what they regularly do to deal with the challenges and frustration of living with their arthritis, a number of great ideas were shared:
One of the most common responses from ACE members was the use of ice and heat, especially in the early days of your disease:
- Ice applied to hot and swollen joints feels good and helps to temporarily reduce inflammation, helping you better recover from exercise sessions.
- Apply moist hot towels to non-inflamed, stiff joints to get ready for activities or exercise.
- Hot and cold baths also help relieve symptoms of joint stiffness and pain.
Sharing your self-care success with your healthcare team
You know your body best and what does – or does not – feel right for you. Trust what your body is telling you and do your best to share those things with your health care team. As mentioned earlier, keeping an arthritis journal is proved to help patients better manage the “details” of their disease, especially with their health care providers.
The aspects of your progress in between visits you need to share with your rheumatologist and other members of your healthcare team (and family and friends if you choose) include:
- An accurate record of prescription medication taking
- Symptoms activity, such as joint pain and stiffness and general feeling of wellness (or fatigue)
- Improvement or limitations in your daily activities, at home and at work
- Questions about changes are additions you would like to make to your treatment goals or treatment plan
- New concerns or fears you may have since your last appointment
|
“You know your body best and what does – or does not – feel right for you. Trust what your body is telling you and do your best to share those things with your health care team.
|
|
Listening to you
We hope you find this information of use. Please tell us what you think by writing to us or emailing us at feedback@jointhealth.org. Through your ongoing and active participation, ACE can make its work more relevant to all Canadians living with arthritis.
Update your email or postal address
Please let us know of any changes by contacting ACE at feedback@jointhealth.org. This will ensure that you continue to receive your free email or print copy of JointHealth™ insight.
Arthritis Consumer Experts (ACE)
Who We Are
Arthritis Consumer Experts (ACE) provides research-based education, advocacy training, advocacy leadership and information to Canadians with arthritis. We help empower people living with all forms of arthritis to take control of their disease and to take action in healthcare and research decision making. ACE activities are guided by its members and led by people with arthritis, leading medical professionals and the ACE Advisory Board. To learn more about ACE, visit: www.jointhealth.org
Acknowledgements
Over the past 12 months, ACE received grants-in-aid from: Amgen Canada, Arthritis Research Canada, AstraZeneca Canada, Canadian Biosimilars Forum, Canadian Institutes of Health Research, Celgene, Eli Lilly Canada, Hoffman-La Roche Canada Ltd., Merck Canada, Novartis, Pfizer Canada, Sandoz Canada, Sanofi Canada, St. Paul’s Hospital (Vancouver), UCB Canada, and the University of British Columbia.
ACE also receives unsolicited donations from its community members (people with arthritis) across Canada.
ACE thanks funders for their support to help the nearly 5 million Canadians living with osteoarthritis, rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis and the many other forms of the disease. ACE assures its members, academic and healthcare professional collaborators, government and the public that the work of ACE is free from influence of its funders.
Disclaimer
The material contained on this website is provided for general information only. This website should not be relied on to suggest a course of treatment for a particular individual or as a substitute for consultation with qualified health professionals who are familiar with your individual medical needs. Should you have any healthcare related questions, you should contact your physician. You should never disregard medical advice or delay in seeking it because of something you have read on this or any website.
This site may provide links to other Internet sites only for the convenience of World Wide Web users. ACE is not responsible for the availability or content of these external sites, nor does ACE endorse, warrant or guarantee the products, services or information described or offered at these other Internet sites.
Although the information presented on this website is believed to be accurate at the time it is posted, this website could include inaccuracies, typographical errors or out-of-date information. This website may be changed at any time without prior notice.
