In this issue
- State of Arthritis Medications:
Some Old, Some New, - Arthritis Medications:
What’s in a Name? - Inside the therapy conversation
- Disease info bytes
- “Cheers” with methotrexate?
JointHealth™ insight Published June 2016

In this Annual issue of JointHealth™, Arthritis Consumer Experts (ACE) presents the 2016 Arthritis Medications Guide, a helpful and trusted tool to understand arthritis medications and the future of arthritis treatment.
The Medications Guide is our attempt to respond to ACE members/patients-at-large who consistently request evidence-based information to enable them to have more meaningful conversations with their rheumatologist and pharmacist around therapy of choice and route of administration. Despite advances in treatment, recent research on treatment response, adherence and preference indicates not all consumers are adequately treated and many remain dissatisfied with their treatment options. For example, high discontinuation rates of biologics were seen in a Canadian cohort of patients with rheumatoid arthritis, according to data presented at the 2014 American College of Rheumatology Annual Meeting.
The Arthritis Medications Guide is intended to help the approximately 600,000 Canadians living with a type of autoimmune arthritis, such as rheumatoid arthritis, ankylosing spondylitis, psoriatic arthritis and juvenile arthritis, understand their treatment options and exercise their right to choose with their healthcare team the therapy best suited to their disease biology, which is distinctly different from patient to patient.
The Arthritis Medications Guide is a companion to ACE’s Annual JointHealth™ Arthritis Medications Report Card - Canada’s only independent patient organization evaluation of public reimbursement access to arthritis medications. In the past year, this landscape has dramatically changed with the public formulary listing of new medications in the biosimilar and targeted synthetic disease-modifying antirheumatic medications category.

When I think about my 27 years of life with rheumatoid arthritis (RA), one thing stands out in terms of how well, or not, I understood and “followed doctor’s orders” when it came to medication taking.
Back in the day, little was known about the differences in understanding between patients and their rheumatologists when it came to “the therapy conversation.” For instance, I would sit on the exam table listening to the rheumatologist’s assessment of my disease at a given point in time and treatment instructions were given to me. But what I heard sounded like it was a foreign language. It wasn’t a conversation between two people; instead, it was me sitting in a small room being talked “at”. This dynamic wasn’t the fault of the rheumatologist, or mine; it’s just the way the rheumatologist-patient relationship worked 20 + years ago. The result at the end of the conversation was that I and my specialist each had a very different understanding about what was decided, what my goals were and what needed to be done and why.
I learned over the course of months and years that I, too, had to speak my rheumatologist’s language, so I went to “RA University” and learned as much about the disease as I possibly could. In fact, I eventually wrote a book about it with Arthritis Research Canada’s scientific director, Dr. John Esdaile. Titled Rheumatoid Arthritis: Plan to Win, the book’s objective is to educate and empower people with RA to be active participants in their healthcare and full partners in decision-making with their healthcare team, and in particular, with their rheumatologist.
Thankfully, health services research over the past two decades has uncovered new information about what’s really going on when we have the therapy conversation with our rheumatologist. Research presented this month at the European League Against Rheumatism scientific meeting shines a light on a number of areas that can be improved in the therapy conversation, such as patients feeling comfortable raising treatment or disease concerns to their rheumatologist and having more medication options to choose from.
Given these emerging data, ACE is developing a new program named JointHealth™ education aimed at helping you, our member, subscriber or reader, with your therapy conversation. It will be launched in September 2016 and designed to engage, educate and empower people like us, people living with arthritis, to be an equal partner in the therapy conversation.
Rheumatoid arthritis is an autoimmune disease where the body’s immune system mistakenly attacks its own healthy joints. The disease process causes swelling and pain in and around joints and can affect the body’s organs including the eyes, lungs, and heart. It is the most common type of inflammatory arthritis and affects approximately 300,000, or 1 in 100, Canadians. It is three times more common in women than it is in men and can occur at any age.
Psoriatic arthritis
Psoriatic arthritis can vary from very mild to very serious. About 150,000 Canadians live with the disease. It is a form of inflammatory arthritis which causes swelling and pain in and around joints, as well as a scaly rash on the skin. It can cause destruction to the peripheral joints as well as the spine. Psoriatic arthritis also affects the tendons and ligaments around the joints. Thirty-percent of patients with psoriasis develop psoriatic arthritis.
Ankylosing spondylitis
Ankylosing spondylitis is a disease primarily affecting the spine but also peripheral joints and tendonous insertions of the bone (enthesitis). About 1 in every 200 people in the population lives with axial and peripheral ankylosing spondylitis. It is three times more common in men than women and commonly begins in teenage or early adult years of life.
Juvenile arthritis
Juvenile arthritis is a childhood disease that causes inflamed and swollen joints due to an overactive immune system that attacks joint tissues. Two common forms of juvenile arthritis include systemic juvenile idiopathic arthritis and polyarticular juvenile idiopathic arthritis. The disease causes pain, fatigue, affects mobility, and can even attack vital organs, such as the eyes. Juvenile arthritis develops in children under the age of 16 years. Approximately 3 in 1000 children in Canada are affected by juvenile arthritis.
Lupus
Lupus is a chronic autoimmune disease. The most common form of lupus is systemic lupus erythematosus, where the body’s immune system malfunctions and attacks normal, healthy tissue, resulting in inflammation, swelling, and damage to joints, skin, kidneys, blood, the heart, and lungs. Lupus affects approximately 1 in 1000 Canadians. For every 9 women, there will be 1 man diagnosed with lupus.

Researchers from the Arthritis Research U.K. Centre for Epidemiology at the University of Manchester have concluded that people with rheumatoid arthritis (RA) currently taking methotrexate are at no greater risk for liver damage than non-drinkers. This is an important finding because some with RA who need to be on and taking methotrexate choose not to take it because they want to enjoy a drink or two throughout their week. But like all things in life, moderation is name of the game.
So how much alcohol can a person with RA drink in a week while on methotrexate without causing worry? UK rheumatologists recommend staying within the limit of 14 units maximum per week.
To learn more about this new research on alcohol intake while taking methotrexate, please visit www.rheumnow.com.
It is important to note that these recommendations may not be appropriate for all RA patients. Speak with your rheumatologist or family physician if you have any question or concerns. And of course, never drink alcohol and drive, and be mindful of other medications you may be taking and their interaction with alcohol.
Listening to you
We hope you find this information of use. Please tell us what you think by writing to us or emailing us at feedback@jointhealth.org. Through your ongoing and active participation, ACE can make its work more relevant to all Canadians living with arthritis.
Update your email or postal address
Please let us know of any changes by contacting ACE at feedback@jointhealth.org. This will ensure that you continue to receive your free email or print copy of JointHealth™ insight.
Arthritis Consumer Experts (ACE)
Who We Are
Arthritis Consumer Experts (ACE) provides research-based education, advocacy training, advocacy leadership and information to Canadians with arthritis. We help empower people living with all forms of arthritis to take control of their disease and to take action in healthcare and research decision making. ACE activities are guided by its members and led by people with arthritis, leading medical professionals and the ACE Advisory Board. To learn more about ACE, visit: www.jointhealth.org
Acknowledgements
Over the past 12 months, ACE received unrestricted grants-in-aid (financial and in-kind) from: AbbVie Corporation, Amgen Canada, Arthritis Research Canada, Canadian Institutes of Health Research, Celgene Inc., Eli Lilly Canada Inc., Hoffman-La Roche Limited, Innovative Medicines Canada, Janssen Inc., Merck Canada Inc., Novartis Pharmaceuticals Canada Inc., Pfizer Canada Inc., Sanofi Canada, St. Paul’s Hospital, UCB Canada Inc. and the University of British Columbia. ACE also receives unsolicited donations from its community members (people with arthritis) across Canada.
ACE’s information, programs and services and opinions are free from influence from individuals or organizations providing ACE unrestricted grant funding.
Disclaimer
The material contained on this website is provided for general information only. This website should not be relied on to suggest a course of treatment for a particular individual or as a substitute for consultation with qualified health professionals who are familiar with your individual medical needs. Should you have any healthcare related questions, you should contact your physician. You should never disregard medical advice or delay in seeking it because of something you have read on this or any website.
This site may provide links to other Internet sites only for the convenience of World Wide Web users. ACE is not responsible for the availability or content of these external sites, nor does ACE endorse, warrant or guarantee the products, services or information described or offered at these other Internet sites.
Although the information presented on this website is believed to be accurate at the time it is posted, this website could include inaccuracies, typographical errors or out-of-date information. This website may be changed at any time without prior notice.

In this Annual issue of JointHealth™, Arthritis Consumer Experts (ACE) presents the 2016 Arthritis Medications Guide, a helpful and trusted tool to understand arthritis medications and the future of arthritis treatment.
The Medications Guide is our attempt to respond to ACE members/patients-at-large who consistently request evidence-based information to enable them to have more meaningful conversations with their rheumatologist and pharmacist around therapy of choice and route of administration. Despite advances in treatment, recent research on treatment response, adherence and preference indicates not all consumers are adequately treated and many remain dissatisfied with their treatment options. For example, high discontinuation rates of biologics were seen in a Canadian cohort of patients with rheumatoid arthritis, according to data presented at the 2014 American College of Rheumatology Annual Meeting.
The Arthritis Medications Guide is intended to help the approximately 600,000 Canadians living with a type of autoimmune arthritis, such as rheumatoid arthritis, ankylosing spondylitis, psoriatic arthritis and juvenile arthritis, understand their treatment options and exercise their right to choose with their healthcare team the therapy best suited to their disease biology, which is distinctly different from patient to patient.
The Arthritis Medications Guide is a companion to ACE’s Annual JointHealth™ Arthritis Medications Report Card - Canada’s only independent patient organization evaluation of public reimbursement access to arthritis medications. In the past year, this landscape has dramatically changed with the public formulary listing of new medications in the biosimilar and targeted synthetic disease-modifying antirheumatic medications category.
Arthritis Medications:
What's in a Name?
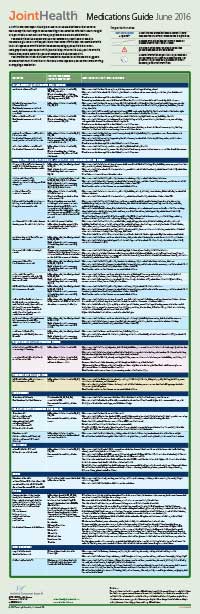
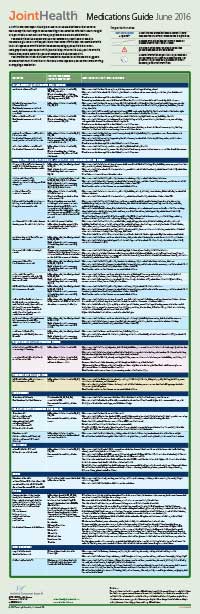
Essentially, there are two categories of medications. It should be noted that the medications in the lower section, (Medications to treat the underlying disease process), are used only in some forms of inflammatory arthritis.
What's in a Name?
Medications to treat symptoms
- non-steroidal anti-inflammatories (NSAIDs)
- pain relievers, like acetaminophen (Tylenol®)
- steroids
- opioids (narcotic)
Glucocorticoids
(GC such as steroids like prednisone): steroids are often used as a “bridging therapy” or to treat life-threatening or organ-threatening complications of rheumatoid arthritis, ankylosing spondylitis, psoriatic arthritis, systemic lupus erythematosus, and vasculitis.
Non–steroidal anti-inflammatory drugs
(NSAIDs such as aspirin, naproxen and celecoxib): these medications help to reduce the inflammation and pain caused by rheumatoid arthritis, ankylosing spondylitis, psoriatic arthritis, and osteoarthritis. Some NSAIDs are available over the counter like ibuprofen (eg. Motrin or Advil) or naproxen (Aleve) while others require a prescription.
Medications to treat the underlying disease
DMARDs, biologic DMARDs,
biosimilar DMARDs, targeted small molecule DMARDs
For many years, rheumatologists have used the term ‘disease-modifying anti-rheumatic drugs’ (DMARDs) to distinguish agents that interfere with the disease process leading to diseases such as rheumatoid arthritis. They alter the natural course of the disease. DMARDs inhibit joint damage, suppress the inflammation, decrease autoantibody levels and have positive effects on long-term functional outcome.
DMARDs now come in all “shapes and sizes” and can be taken by pill, self-injection and infusion (IV). Each DMARD works in a unique way and the decision about which one(s) is best for you is perhaps the most important conversation you can have with your rheumatologists.
biosimilar DMARDs, targeted small molecule DMARDs
For many years, rheumatologists have used the term ‘disease-modifying anti-rheumatic drugs’ (DMARDs) to distinguish agents that interfere with the disease process leading to diseases such as rheumatoid arthritis. They alter the natural course of the disease. DMARDs inhibit joint damage, suppress the inflammation, decrease autoantibody levels and have positive effects on long-term functional outcome.
DMARDs now come in all “shapes and sizes” and can be taken by pill, self-injection and infusion (IV). Each DMARD works in a unique way and the decision about which one(s) is best for you is perhaps the most important conversation you can have with your rheumatologists.
In light of the recent emergence of new classes of treatment for the different forms of inflammatory arthritis, such as biosimilars and Janus kinase (JAK) inhibitors, a new naming system for disease-modifying antirheumatic drugs (DMARDs) is being adopted in Europe and North America. In this new system, there are classifications for:
Synthetic (or chemical) DMARDs are now divided into:
csDMARDs: Conventional synthetic DMARDs include traditional medications such as methotrexate, sulfasalazine, leflunomide, hydroxychloroquine, gold salts and others.
tsDMARDs: Targeted synthetic DMARDs include only those medications that were specifically developed to target a particular molecular structure such as tofacitinib, baricitinib or apremilast, or agents not focused primarily on rheumatic diseases, such as imatinib or ibrutinib.
csDMARDs: Conventional synthetic DMARDs include traditional medications such as methotrexate, sulfasalazine, leflunomide, hydroxychloroquine, gold salts and others.
tsDMARDs: Targeted synthetic DMARDs include only those medications that were specifically developed to target a particular molecular structure such as tofacitinib, baricitinib or apremilast, or agents not focused primarily on rheumatic diseases, such as imatinib or ibrutinib.
Biological DMARDs are now divided into:
boDMARDS: Biological original DMARDs include abatacept, adalimumab, anakinra, certolizumab pegol, etanercept, golimumab, infliximab-Remicade, rituximab or tocilizumab.
bsDMARDs: Biosimilar DMARDs include infliximab-Inflectra
boDMARDS: Biological original DMARDs include abatacept, adalimumab, anakinra, certolizumab pegol, etanercept, golimumab, infliximab-Remicade, rituximab or tocilizumab.
bsDMARDs: Biosimilar DMARDs include infliximab-Inflectra
Inside the therapy conversation
by Cheryl Koehn, Founder and President, Arthritis Consumer Experts
When I think about my 27 years of life with rheumatoid arthritis (RA), one thing stands out in terms of how well, or not, I understood and “followed doctor’s orders” when it came to medication taking.
Back in the day, little was known about the differences in understanding between patients and their rheumatologists when it came to “the therapy conversation.” For instance, I would sit on the exam table listening to the rheumatologist’s assessment of my disease at a given point in time and treatment instructions were given to me. But what I heard sounded like it was a foreign language. It wasn’t a conversation between two people; instead, it was me sitting in a small room being talked “at”. This dynamic wasn’t the fault of the rheumatologist, or mine; it’s just the way the rheumatologist-patient relationship worked 20 + years ago. The result at the end of the conversation was that I and my specialist each had a very different understanding about what was decided, what my goals were and what needed to be done and why.
I learned over the course of months and years that I, too, had to speak my rheumatologist’s language, so I went to “RA University” and learned as much about the disease as I possibly could. In fact, I eventually wrote a book about it with Arthritis Research Canada’s scientific director, Dr. John Esdaile. Titled Rheumatoid Arthritis: Plan to Win, the book’s objective is to educate and empower people with RA to be active participants in their healthcare and full partners in decision-making with their healthcare team, and in particular, with their rheumatologist.
Thankfully, health services research over the past two decades has uncovered new information about what’s really going on when we have the therapy conversation with our rheumatologist. Research presented this month at the European League Against Rheumatism scientific meeting shines a light on a number of areas that can be improved in the therapy conversation, such as patients feeling comfortable raising treatment or disease concerns to their rheumatologist and having more medication options to choose from.
Given these emerging data, ACE is developing a new program named JointHealth™ education aimed at helping you, our member, subscriber or reader, with your therapy conversation. It will be launched in September 2016 and designed to engage, educate and empower people like us, people living with arthritis, to be an equal partner in the therapy conversation.
Disease info bytes
Rheumatoid arthritisRheumatoid arthritis is an autoimmune disease where the body’s immune system mistakenly attacks its own healthy joints. The disease process causes swelling and pain in and around joints and can affect the body’s organs including the eyes, lungs, and heart. It is the most common type of inflammatory arthritis and affects approximately 300,000, or 1 in 100, Canadians. It is three times more common in women than it is in men and can occur at any age.
Psoriatic arthritis
Psoriatic arthritis can vary from very mild to very serious. About 150,000 Canadians live with the disease. It is a form of inflammatory arthritis which causes swelling and pain in and around joints, as well as a scaly rash on the skin. It can cause destruction to the peripheral joints as well as the spine. Psoriatic arthritis also affects the tendons and ligaments around the joints. Thirty-percent of patients with psoriasis develop psoriatic arthritis.
Ankylosing spondylitis
Ankylosing spondylitis is a disease primarily affecting the spine but also peripheral joints and tendonous insertions of the bone (enthesitis). About 1 in every 200 people in the population lives with axial and peripheral ankylosing spondylitis. It is three times more common in men than women and commonly begins in teenage or early adult years of life.
Juvenile arthritis
Juvenile arthritis is a childhood disease that causes inflamed and swollen joints due to an overactive immune system that attacks joint tissues. Two common forms of juvenile arthritis include systemic juvenile idiopathic arthritis and polyarticular juvenile idiopathic arthritis. The disease causes pain, fatigue, affects mobility, and can even attack vital organs, such as the eyes. Juvenile arthritis develops in children under the age of 16 years. Approximately 3 in 1000 children in Canada are affected by juvenile arthritis.
Lupus
Lupus is a chronic autoimmune disease. The most common form of lupus is systemic lupus erythematosus, where the body’s immune system malfunctions and attacks normal, healthy tissue, resulting in inflammation, swelling, and damage to joints, skin, kidneys, blood, the heart, and lungs. Lupus affects approximately 1 in 1000 Canadians. For every 9 women, there will be 1 man diagnosed with lupus.
“Cheers” with methotrexate?

Researchers from the Arthritis Research U.K. Centre for Epidemiology at the University of Manchester have concluded that people with rheumatoid arthritis (RA) currently taking methotrexate are at no greater risk for liver damage than non-drinkers. This is an important finding because some with RA who need to be on and taking methotrexate choose not to take it because they want to enjoy a drink or two throughout their week. But like all things in life, moderation is name of the game.
So how much alcohol can a person with RA drink in a week while on methotrexate without causing worry? UK rheumatologists recommend staying within the limit of 14 units maximum per week.

|

|

|

|
|
Wine (13%) 6 175ml Glasses |
Lager or Ale (4%) 6 568ml Pints |
Cider (4.5%) 6 568ml Pints |
Spirits (40%) 6 25ml Glasses |
To learn more about this new research on alcohol intake while taking methotrexate, please visit www.rheumnow.com.
It is important to note that these recommendations may not be appropriate for all RA patients. Speak with your rheumatologist or family physician if you have any question or concerns. And of course, never drink alcohol and drive, and be mindful of other medications you may be taking and their interaction with alcohol.
Listening to you
We hope you find this information of use. Please tell us what you think by writing to us or emailing us at feedback@jointhealth.org. Through your ongoing and active participation, ACE can make its work more relevant to all Canadians living with arthritis.
Update your email or postal address
Please let us know of any changes by contacting ACE at feedback@jointhealth.org. This will ensure that you continue to receive your free email or print copy of JointHealth™ insight.
Arthritis Consumer Experts (ACE)
Who We Are
Arthritis Consumer Experts (ACE) provides research-based education, advocacy training, advocacy leadership and information to Canadians with arthritis. We help empower people living with all forms of arthritis to take control of their disease and to take action in healthcare and research decision making. ACE activities are guided by its members and led by people with arthritis, leading medical professionals and the ACE Advisory Board. To learn more about ACE, visit: www.jointhealth.org
Acknowledgements
Over the past 12 months, ACE received unrestricted grants-in-aid (financial and in-kind) from: AbbVie Corporation, Amgen Canada, Arthritis Research Canada, Canadian Institutes of Health Research, Celgene Inc., Eli Lilly Canada Inc., Hoffman-La Roche Limited, Innovative Medicines Canada, Janssen Inc., Merck Canada Inc., Novartis Pharmaceuticals Canada Inc., Pfizer Canada Inc., Sanofi Canada, St. Paul’s Hospital, UCB Canada Inc. and the University of British Columbia. ACE also receives unsolicited donations from its community members (people with arthritis) across Canada.
ACE’s information, programs and services and opinions are free from influence from individuals or organizations providing ACE unrestricted grant funding.
Disclaimer
The material contained on this website is provided for general information only. This website should not be relied on to suggest a course of treatment for a particular individual or as a substitute for consultation with qualified health professionals who are familiar with your individual medical needs. Should you have any healthcare related questions, you should contact your physician. You should never disregard medical advice or delay in seeking it because of something you have read on this or any website.
This site may provide links to other Internet sites only for the convenience of World Wide Web users. ACE is not responsible for the availability or content of these external sites, nor does ACE endorse, warrant or guarantee the products, services or information described or offered at these other Internet sites.
Although the information presented on this website is believed to be accurate at the time it is posted, this website could include inaccuracies, typographical errors or out-of-date information. This website may be changed at any time without prior notice.

