In this issue
- Arthritis Research Update:
The ACE Report - New Guideline for the Treatment of RA
- "Treat-to-Target": A consumer definition
- Methotrexate Matters in RA
- Looking for ANSWERS
- SEB Facts
- New Promising Lupus Therapies and Insights
JointHealth™ insight Published May 2016



An important job each year for Arthritis Consumer Experts (ACE) is to monitor and deliver straight to your inbox some of what is new and upcoming in the global arthritis research community. Our attendance at the Annual Scientific Meetings of the American College of Rheumatology and Association of Rheumatology Health Professionals (ACR/ARHP) each year enables us to maintain the high quality information we write about and bring to you now, and throughout each year.
At the November 2015 meeting, 16,000 basic and clinical researchers in rheumatology and immunology gathered from around the world to share and discuss the latest science on arthritis causes, treatments, care and healthcare system and societal costs. So in this special 2016 issue of JointHealth™ insight, we give you an inside look at research advances from the ACE perspective.
Each year the ACR/AHRP recognizes excellence in its communities at their annual meeting. At its recent meeting, several of our Canadian rheumatology community leaders received prestigious awards. Congratulations to one and all.

Dr. Linda Li, PT, MSc, PhD, from Arthritis Research Canada, received the ARHP Distinguished Scholar Award, presented to an individual who demonstrates exceptional achievements in scholarly activities pertinent to arthritis and the rheumatic diseases.

Dr. Paul Adam, MSW, from the Mary Pack Arthritis Centre, received the President’s Award, presented to the ARHP/ACR member or team performing outstanding service within the present year in advancing the goals, ideals, and standards of ARHP.
Recognition as a Master of the American College of Rheumatology is one of the highest honours the ACR bestows on a member. This distinction is given to members age 65 or older who have made outstanding contributions to the field of rheumatology through scholarly achievement and/or service to their patients, students, and profession. Since 1987, the ACR has honoured more than 300 exceptional leaders in the field of rheumatology as Masters. This year, the ACR recognized several Canadian physicians:
Robert Inman, MD
Professor of Medicine and Immunology, University of Toronto, Deputy Physician in Chief, Research, University Health Network, Director, Spondylitis Program, Toronto Western Hospital, Senior Scientist, Toronto Western Research Institute.
Kiem Oen, MD
Professor, Department of Pediatrics and Child Health, University of Manitoba.
Alan Rosenberg, MD, FRCPC Professor, Department of Pediatrics, College of Medicine, University of Saskatchewan
New Guideline for the Treatment of RA
The American College of Rheumatology (ACR) released its Guideline for the Treatment of Rheumatoid Arthritis (RA) during the ACR/ARHP Annual Meeting and now available on the ACR website. The ACR plans to develop a pocket card, an app version of the guideline and a patient education tool to help promote the guideline with both patients and healthcare providers.
The guideline includes recommendations intended to align understanding between patients and physicians about what the best course of action for their care should be, based on the science, including:

"Treat-to-Target": A consumer definition
If you pick up a medical magazine for arthritis professionals these days, you often see the phrase “treat-to-target” among the pages. It is a phrase that describes a relatively new approach to the treatment of inflammatory forms of arthritis, such as RA.
The goal of the treat-to-target approach is for rheumatologists to aim to put their patient’s disease into remission – in other words, remission becomes the “bulls-eye” of the treatment target.
What does that mean for patients? It means they should be nearly, or completely, free of inflammation, pain and other hallmark symptoms of this group of diseases. Central to this treatment philosophy is aggressively starting medications after diagnosis and if necessary changing them every two or three months until a therapy combination brings the disease under maximal control.
From a patient point-of-view, the treat-to-target approach may seem like trial and error, but because there are no diagnostic tests available which guide them in which medication(s) will work in each and every patient, rheumatologists usually start a person on methotrexate at a dose of between 15 – 25 mg, and if inflammation is still present after 6 weeks, they add one or two other disease modifying anti-rheumatic drugs.
The majority of rheumatologists in Canada, the United States and Europe are now taking this approach with their inflammatory arthritis patients.
Methotrexate Matters in RA
Disease-modifying anti-rheumatic drugs (DMARDs), such as methotrexate, can substantially reduce the inflammation of rheumatoid arthritis, reduce or prevent joint damage, preserve joint structure and function, and enable a patient to continue his or her daily activities. Although some DMARDs take time to fully work, they may allow you to take a lower dose of glucocorticoids (also called “steroids”) to control pain and inflammation.
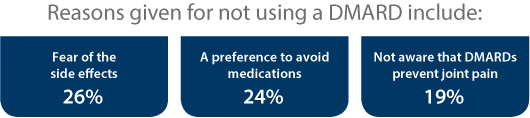
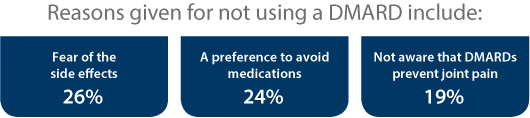
For people with RA, DMARDs should be used within the first three months of symptoms in order to prevent permanent joint damage. However, a 2007 study by Dr. Diane Lacaille found a long delay in DMARD use in British Columbia. Only 33% of the 1,822 people with RA surveyed had begun taking DMARDs.
This delay in DMARD use means patients not taking these medications in a timely manner are actually increasing their risk of joint damage, disability and even premature death.
According to research presented at the ACR Annual Meeting, methotrexate is being prescribed to patients with rheumatoid arthritis at too low doses, for an inadequate length of time and rarely switched to subcutaneous (under the skin injection) before rheumatologists move on to biologic therapy based on an analysis of claims data from 35,640 rheumatoid arthritis patients in the U.S.
“There are some major concerns here. Methotrexate is the anchor drug for rheumatoid arthritis, the best drug we have. More appropriate [use] could lead to better control” and “produce significant cost savings,” said lead researcher Dr. James O’Dell, chief of the division of rheumatology at the University of Nebraska Medical Center, Omaha.
Looking for
ANSWERS
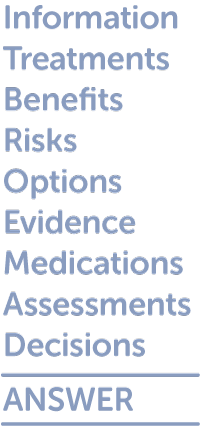 To help people with rheumatoid arthritis learn about methotrexate and help them decide if it’s the right medication for them, Dr. Linda Li, Senior Scientist at Arthritis Research Canada (ARC), has developed a decision aid for people with RA called ANSWER (Animated Self-serve Web-based Research) that combines the best scientific evidence with ‘real-world’ information.
To help people with rheumatoid arthritis learn about methotrexate and help them decide if it’s the right medication for them, Dr. Linda Li, Senior Scientist at Arthritis Research Canada (ARC), has developed a decision aid for people with RA called ANSWER (Animated Self-serve Web-based Research) that combines the best scientific evidence with ‘real-world’ information.
According to Dr. Li, the ANSWER program can:
New Data on SEBs
One of the hot topics at the ACR Annual Meeting was subsequent entry biologics, or biosimiliars, as they are called in the U.S. At the meeting, there were a number of presentations of phase 3 studies of biosimilar molecules of adalimumab, etanercept, and infliximab—back to back, with very a similar trial design of looking at early time points—which are very sensitive parts of the study—to assess biosimilarity. The collective results showed successful demonstration of the same efficacy and safety across three different SEB molecules as the originator molecules in patients with rheumatoid arthritis who did not respond to methotrexate.
 Together, the meeting presentations confirmed for the rheumatology community that SEBs/biosimiliars can potentially provide people with inflammatory arthritis and the healthcare system effective therapies at a lower cost.
Together, the meeting presentations confirmed for the rheumatology community that SEBs/biosimiliars can potentially provide people with inflammatory arthritis and the healthcare system effective therapies at a lower cost.
Following the annual conference, the Food and Drug Administration (FDA) announced on April 5, 2016, the approval of infliximab (Inflectra), the first biosimilar to receive approval in the U.S. for the treatment of rheumatic diseases, including rheumatoid arthritis and psoriatic arthritis.
Commenting on the news, Joan Von Feldt, MD, MSEd, President of the American College of Rheumatology said:
“The safe adoption of biosimilars into the U.S. marketplace remains a top priority for the American College of Rheumatology. Biologics are a lifeline for patients living with rheumatic disease, helping many to avoid pain, long-term disability, and life-threatening complications. Unfortunately, many of our patients struggle to afford these complex therapies due to their high cost.
“The ACR welcomes the introduction of biosimilars to the U.S. healthcare system and is hopeful that the decrease in cost resulting from the availability of safe and effective biosimilars in the U.S. will increase our patients’ access to life-changing therapies and improve their overall health.“
SEBs in Canada: An ACE Update
Canada’s 600,000 patients living with inflammatory arthritis are on the frontline of the entry of SEBS.
Provincial formularies and private health insurers have begun providing reimbursement listing for the first SEB approved in Canada. Both public and private payers are considering SEBs as a key element in their mandates to list cost-effective drug treatment that are both clinically meaningful to patients and conducive to long-term cost reductions and drug plan sustainability.
SEBs offer patients and physicians an additional new choice in the treatment of inflammatory arthritis at a reduced price from the originator biologic.
As SEB research data continues to be published and SEB policies evolve, ACE is meeting with provincial formulary and private payer decision makers and advocating for the introduction of SEBs in a manner that respects the integrity of the patient-doctor relationship and ability to choose the best therapy for their disease and not to force stable patients on current therapies to an SEB, given not enough evidence exists to show this is a safe and effective practice.
ACE is also advocating that if governments want to put patients first and achieve significant levels of total drug plan savings, then SEBs represent an opportunity to save money and reinvest in patient care and innovative therapies arriving in the marketplace proven to be safe, effective and cost effective for healthcare systems.
ACE has consistently recommended governments reinvest the savings from SEB price reductions back to formulary budgets so that new Health Canada-approved therapies can be listed on the provincial formulary much more quickly, if supported by the science and arthritis community, to the benefit of Canada’s 600,000 people living with inflammatory arthritis.
How can you stay informed and involved?

SEBs will have an increasing role to play in the Canadian health system. How can you stay informed and involved?
New Promising Lupus Therapies and Insights
At a Novel Therapies in Lupus session at the recent ACR Annual Meeting, data on a biologic, belimumab, was presented during this session. Belimumab is the first drug approved to treat lupus in more than 50 years and is the first drug developed specifically for lupus. However, a recent multi-center, international phase III trial looked at a new way to deliver the drug—via subcutaneous (under the skin) injection.
Currently, belimumab must be administered by a medical professional through an intravenous infusion directly into the vein. However, subcutaneous injection of belimumab has the potential to be self-administered, which could enhance treatment options for people with lupus. In the trial, participants who received belimumab through injection plus standard of care medications had significantly greater reductions in disease activity compared to the placebo group. In addition, when compared to data from previous belimumab trials, belimumab delivered by injection seems to be as effective at reducing disease activity as the intravenous method.
Lupus and Pregnancy
For years doctors have been advising patients with lupus not to get pregnant. It was assumed that the likelihood of pregnancy complications was too high in this population. However, ongoing work by U.S. researchers is helping identify those lupus patients who are – and are not – at increased risk of problem pregnancies.
The research, being led by Jane E. Salmon, MD, Director of the Lupus and APS Center of Excellence at Hospital for Special Surgery, is part of the PROMISSE Study, or “Predicators of pRegnacy Outcome: BioMarkers in antiphospholipid antibody Syndrome and System lupus Erythematosus.”
 At this year’s ACR Annual Meeting, Dr. Salmon presented new PROMISSE data showing that complement activation is a strong predictor of adverse pregnancy outcomes, including fetal/neonatal death, pre-term delivery, and marked growth restriction.
At this year’s ACR Annual Meeting, Dr. Salmon presented new PROMISSE data showing that complement activation is a strong predictor of adverse pregnancy outcomes, including fetal/neonatal death, pre-term delivery, and marked growth restriction.
“PROMISSE is the first study of its size and detail to assess complement activation throughout pregnancy,” explains Salmon. “By harnessing the resources of PROMISSE, we have identified another early marker that signals a possible adverse pregnancy. Our team has successfully defined a collection of biomarkers which we are now poised to combine to have an even greater ability to risk-stratify patients.”
Identification of those women likely to have safe, uncomplicated pregnancies with biomarkers, including products of complement activation, along with clinical risk factors, would enable physicians to reassure low-risk mothers that their pregnancies should progress normally, and reduce the need for extensive medical evaluations, visits, and costs. Conversely, patients identified as being at high risk could be more diligently monitored.
Listening to you
We hope you find this information of use. Please tell us what you think by writing to us or emailing us at feedback@jointhealth.org. Through your ongoing and active participation, ACE can make its work more relevant to all Canadians living with arthritis.
Update your email or postal address
Please let us know of any changes by contacting ACE at feedback@jointhealth.org. This will ensure that you continue to receive your free email or print copy of JointHealth™ insight.
Arthritis Consumer Experts (ACE)
Who We Are
Arthritis Consumer Experts (ACE) provides research-based education, advocacy training, advocacy leadership and information to Canadians with arthritis. We help empower people living with all forms of arthritis to take control of their disease and to take action in healthcare and research decision making. ACE activities are guided by its members and led by people with arthritis, leading medical professionals and the ACE Advisory Board. To learn more about ACE, visit: www.jointhealth.org
Acknowledgements
Over the past 12 months, ACE received unrestricted grants-in-aid (financial and in-kind) from: AbbVie Corporation, Amgen Canada, Arthritis Research Canada, Canadian Institutes of Health Research, Celgene Inc., Eli Lilly Canada Inc., Hoffman-La Roche Limited, Innovative Medicines Canada, Janssen Inc., Merck Canada Inc., Novartis Pharmaceuticals Canada Inc., Pfizer Canada Inc., Sanofi Canada, St. Paul’s Hospital, UCB Canada Inc. and the University of British Columbia. ACE also receives unsolicited donations from its community members (people with arthritis) across Canada.
ACE’s information, programs and services and opinions are free from influence from individuals or organizations providing ACE unrestricted grant funding.
Disclaimer
The material contained on this website is provided for general information only. This website should not be relied on to suggest a course of treatment for a particular individual or as a substitute for consultation with qualified health professionals who are familiar with your individual medical needs. Should you have any healthcare related questions, you should contact your physician. You should never disregard medical advice or delay in seeking it because of something you have read on this or any website.
This site may provide links to other Internet sites only for the convenience of World Wide Web users. ACE is not responsible for the availability or content of these external sites, nor does ACE endorse, warrant or guarantee the products, services or information described or offered at these other Internet sites.
Although the information presented on this website is believed to be accurate at the time it is posted, this website could include inaccuracies, typographical errors or out-of-date information. This website may be changed at any time without prior notice.



An important job each year for Arthritis Consumer Experts (ACE) is to monitor and deliver straight to your inbox some of what is new and upcoming in the global arthritis research community. Our attendance at the Annual Scientific Meetings of the American College of Rheumatology and Association of Rheumatology Health Professionals (ACR/ARHP) each year enables us to maintain the high quality information we write about and bring to you now, and throughout each year.
At the November 2015 meeting, 16,000 basic and clinical researchers in rheumatology and immunology gathered from around the world to share and discuss the latest science on arthritis causes, treatments, care and healthcare system and societal costs. So in this special 2016 issue of JointHealth™ insight, we give you an inside look at research advances from the ACE perspective.
Each year the ACR/AHRP recognizes excellence in its communities at their annual meeting. At its recent meeting, several of our Canadian rheumatology community leaders received prestigious awards. Congratulations to one and all.

Dr. Linda Li, PT, MSc, PhD, from Arthritis Research Canada, received the ARHP Distinguished Scholar Award, presented to an individual who demonstrates exceptional achievements in scholarly activities pertinent to arthritis and the rheumatic diseases.

Dr. Paul Adam, MSW, from the Mary Pack Arthritis Centre, received the President’s Award, presented to the ARHP/ACR member or team performing outstanding service within the present year in advancing the goals, ideals, and standards of ARHP.
Recognition as a Master of the American College of Rheumatology is one of the highest honours the ACR bestows on a member. This distinction is given to members age 65 or older who have made outstanding contributions to the field of rheumatology through scholarly achievement and/or service to their patients, students, and profession. Since 1987, the ACR has honoured more than 300 exceptional leaders in the field of rheumatology as Masters. This year, the ACR recognized several Canadian physicians:
Robert Inman, MD
Professor of Medicine and Immunology, University of Toronto, Deputy Physician in Chief, Research, University Health Network, Director, Spondylitis Program, Toronto Western Hospital, Senior Scientist, Toronto Western Research Institute.
Kiem Oen, MD
Professor, Department of Pediatrics and Child Health, University of Manitoba.
Alan Rosenberg, MD, FRCPC Professor, Department of Pediatrics, College of Medicine, University of Saskatchewan
New Guideline for the Treatment of RA
The American College of Rheumatology (ACR) released its Guideline for the Treatment of Rheumatoid Arthritis (RA) during the ACR/ARHP Annual Meeting and now available on the ACR website. The ACR plans to develop a pocket card, an app version of the guideline and a patient education tool to help promote the guideline with both patients and healthcare providers.
The guideline includes recommendations intended to align understanding between patients and physicians about what the best course of action for their care should be, based on the science, including:
- The use of disease-modifying anti-rheumatic drugs (DMARDs), biologics, tofacitinib and glucocorticoids in patients with early RA (less than six months) and established RA (six months or more),
- Recommendations on using a “treat-to-target” approach, tapering and discontinuing medications;
- The use of biologics and DMARDs in RA patients who also have other chronic or serious illnesses or diseases (e.g. hepatitis, congestive heart failure, malignancy and serious infections);
- The use of vaccines in patients starting/receiving DMARDs or biologics;
- Screening for tuberculosis in patients starting/receiving biologics or tofacitinib; and
- Regular blood test monitoring for traditional DMARDs.

"Treat-to-Target": A consumer definition
If you pick up a medical magazine for arthritis professionals these days, you often see the phrase “treat-to-target” among the pages. It is a phrase that describes a relatively new approach to the treatment of inflammatory forms of arthritis, such as RA.
The goal of the treat-to-target approach is for rheumatologists to aim to put their patient’s disease into remission – in other words, remission becomes the “bulls-eye” of the treatment target.
What does that mean for patients? It means they should be nearly, or completely, free of inflammation, pain and other hallmark symptoms of this group of diseases. Central to this treatment philosophy is aggressively starting medications after diagnosis and if necessary changing them every two or three months until a therapy combination brings the disease under maximal control.
From a patient point-of-view, the treat-to-target approach may seem like trial and error, but because there are no diagnostic tests available which guide them in which medication(s) will work in each and every patient, rheumatologists usually start a person on methotrexate at a dose of between 15 – 25 mg, and if inflammation is still present after 6 weeks, they add one or two other disease modifying anti-rheumatic drugs.
The majority of rheumatologists in Canada, the United States and Europe are now taking this approach with their inflammatory arthritis patients.
Methotrexate Matters in RA
Disease-modifying anti-rheumatic drugs (DMARDs), such as methotrexate, can substantially reduce the inflammation of rheumatoid arthritis, reduce or prevent joint damage, preserve joint structure and function, and enable a patient to continue his or her daily activities. Although some DMARDs take time to fully work, they may allow you to take a lower dose of glucocorticoids (also called “steroids”) to control pain and inflammation.
For people with RA, DMARDs should be used within the first three months of symptoms in order to prevent permanent joint damage. However, a 2007 study by Dr. Diane Lacaille found a long delay in DMARD use in British Columbia. Only 33% of the 1,822 people with RA surveyed had begun taking DMARDs.
This delay in DMARD use means patients not taking these medications in a timely manner are actually increasing their risk of joint damage, disability and even premature death.
According to research presented at the ACR Annual Meeting, methotrexate is being prescribed to patients with rheumatoid arthritis at too low doses, for an inadequate length of time and rarely switched to subcutaneous (under the skin injection) before rheumatologists move on to biologic therapy based on an analysis of claims data from 35,640 rheumatoid arthritis patients in the U.S.
“There are some major concerns here. Methotrexate is the anchor drug for rheumatoid arthritis, the best drug we have. More appropriate [use] could lead to better control” and “produce significant cost savings,” said lead researcher Dr. James O’Dell, chief of the division of rheumatology at the University of Nebraska Medical Center, Omaha.
Looking for
ANSWERS
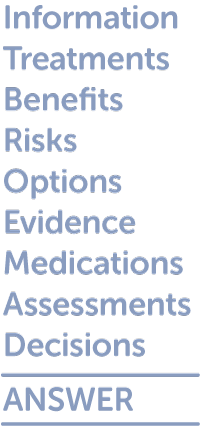 To help people with rheumatoid arthritis learn about methotrexate and help them decide if it’s the right medication for them, Dr. Linda Li, Senior Scientist at Arthritis Research Canada (ARC), has developed a decision aid for people with RA called ANSWER (Animated Self-serve Web-based Research) that combines the best scientific evidence with ‘real-world’ information.
To help people with rheumatoid arthritis learn about methotrexate and help them decide if it’s the right medication for them, Dr. Linda Li, Senior Scientist at Arthritis Research Canada (ARC), has developed a decision aid for people with RA called ANSWER (Animated Self-serve Web-based Research) that combines the best scientific evidence with ‘real-world’ information.According to Dr. Li, the ANSWER program can:
- Improve understanding of benefits and risks of different treatment options
- Provide user-friendly information based on best evidence of management options in early RA. This information is presented side by side with medication options that the individual may want to discuss with their doctor.
- Facilitate decision-making in the context of your everyday life. The ANSWER program assists individuals to assess and reflect upon the ways in which the information provided may be personally relevant, harmful or beneficial.
- ANSWER is designed to help people with early RA make informed, timely decisions about whether or not to use the DMARD, Methotrexate.
New Data on SEBs
One of the hot topics at the ACR Annual Meeting was subsequent entry biologics, or biosimiliars, as they are called in the U.S. At the meeting, there were a number of presentations of phase 3 studies of biosimilar molecules of adalimumab, etanercept, and infliximab—back to back, with very a similar trial design of looking at early time points—which are very sensitive parts of the study—to assess biosimilarity. The collective results showed successful demonstration of the same efficacy and safety across three different SEB molecules as the originator molecules in patients with rheumatoid arthritis who did not respond to methotrexate.
 Together, the meeting presentations confirmed for the rheumatology community that SEBs/biosimiliars can potentially provide people with inflammatory arthritis and the healthcare system effective therapies at a lower cost.
Together, the meeting presentations confirmed for the rheumatology community that SEBs/biosimiliars can potentially provide people with inflammatory arthritis and the healthcare system effective therapies at a lower cost.Following the annual conference, the Food and Drug Administration (FDA) announced on April 5, 2016, the approval of infliximab (Inflectra), the first biosimilar to receive approval in the U.S. for the treatment of rheumatic diseases, including rheumatoid arthritis and psoriatic arthritis.
Commenting on the news, Joan Von Feldt, MD, MSEd, President of the American College of Rheumatology said:
“The safe adoption of biosimilars into the U.S. marketplace remains a top priority for the American College of Rheumatology. Biologics are a lifeline for patients living with rheumatic disease, helping many to avoid pain, long-term disability, and life-threatening complications. Unfortunately, many of our patients struggle to afford these complex therapies due to their high cost.
“The ACR welcomes the introduction of biosimilars to the U.S. healthcare system and is hopeful that the decrease in cost resulting from the availability of safe and effective biosimilars in the U.S. will increase our patients’ access to life-changing therapies and improve their overall health.“
SEBs in Canada: An ACE Update
Canada’s 600,000 patients living with inflammatory arthritis are on the frontline of the entry of SEBS.
Provincial formularies and private health insurers have begun providing reimbursement listing for the first SEB approved in Canada. Both public and private payers are considering SEBs as a key element in their mandates to list cost-effective drug treatment that are both clinically meaningful to patients and conducive to long-term cost reductions and drug plan sustainability.
SEBs offer patients and physicians an additional new choice in the treatment of inflammatory arthritis at a reduced price from the originator biologic.
As SEB research data continues to be published and SEB policies evolve, ACE is meeting with provincial formulary and private payer decision makers and advocating for the introduction of SEBs in a manner that respects the integrity of the patient-doctor relationship and ability to choose the best therapy for their disease and not to force stable patients on current therapies to an SEB, given not enough evidence exists to show this is a safe and effective practice.
ACE is also advocating that if governments want to put patients first and achieve significant levels of total drug plan savings, then SEBs represent an opportunity to save money and reinvest in patient care and innovative therapies arriving in the marketplace proven to be safe, effective and cost effective for healthcare systems.
ACE has consistently recommended governments reinvest the savings from SEB price reductions back to formulary budgets so that new Health Canada-approved therapies can be listed on the provincial formulary much more quickly, if supported by the science and arthritis community, to the benefit of Canada’s 600,000 people living with inflammatory arthritis.
How can you stay informed and involved?

SEBs will have an increasing role to play in the Canadian health system. How can you stay informed and involved?
- Provide your comments and questions to Arthritis Consumer Experts at feedback@jointhealth.org
- Stay informed and seek out “lay language”, research-based information about SEBs by visiting the JointHealth™ shareables page here.
- Continue to share perspectives and experiences around this important health topic
- Help educate your community – they will be affected by the arrival of SEBs
- Understand how SEBs are assessed and listed on public and private formularies
New Promising Lupus Therapies and Insights
At a Novel Therapies in Lupus session at the recent ACR Annual Meeting, data on a biologic, belimumab, was presented during this session. Belimumab is the first drug approved to treat lupus in more than 50 years and is the first drug developed specifically for lupus. However, a recent multi-center, international phase III trial looked at a new way to deliver the drug—via subcutaneous (under the skin) injection.
Currently, belimumab must be administered by a medical professional through an intravenous infusion directly into the vein. However, subcutaneous injection of belimumab has the potential to be self-administered, which could enhance treatment options for people with lupus. In the trial, participants who received belimumab through injection plus standard of care medications had significantly greater reductions in disease activity compared to the placebo group. In addition, when compared to data from previous belimumab trials, belimumab delivered by injection seems to be as effective at reducing disease activity as the intravenous method.
Lupus and Pregnancy
For years doctors have been advising patients with lupus not to get pregnant. It was assumed that the likelihood of pregnancy complications was too high in this population. However, ongoing work by U.S. researchers is helping identify those lupus patients who are – and are not – at increased risk of problem pregnancies.
The research, being led by Jane E. Salmon, MD, Director of the Lupus and APS Center of Excellence at Hospital for Special Surgery, is part of the PROMISSE Study, or “Predicators of pRegnacy Outcome: BioMarkers in antiphospholipid antibody Syndrome and System lupus Erythematosus.”
 At this year’s ACR Annual Meeting, Dr. Salmon presented new PROMISSE data showing that complement activation is a strong predictor of adverse pregnancy outcomes, including fetal/neonatal death, pre-term delivery, and marked growth restriction.
At this year’s ACR Annual Meeting, Dr. Salmon presented new PROMISSE data showing that complement activation is a strong predictor of adverse pregnancy outcomes, including fetal/neonatal death, pre-term delivery, and marked growth restriction.“PROMISSE is the first study of its size and detail to assess complement activation throughout pregnancy,” explains Salmon. “By harnessing the resources of PROMISSE, we have identified another early marker that signals a possible adverse pregnancy. Our team has successfully defined a collection of biomarkers which we are now poised to combine to have an even greater ability to risk-stratify patients.”
Identification of those women likely to have safe, uncomplicated pregnancies with biomarkers, including products of complement activation, along with clinical risk factors, would enable physicians to reassure low-risk mothers that their pregnancies should progress normally, and reduce the need for extensive medical evaluations, visits, and costs. Conversely, patients identified as being at high risk could be more diligently monitored.
Listening to you
We hope you find this information of use. Please tell us what you think by writing to us or emailing us at feedback@jointhealth.org. Through your ongoing and active participation, ACE can make its work more relevant to all Canadians living with arthritis.
Update your email or postal address
Please let us know of any changes by contacting ACE at feedback@jointhealth.org. This will ensure that you continue to receive your free email or print copy of JointHealth™ insight.
Arthritis Consumer Experts (ACE)
Who We Are
Arthritis Consumer Experts (ACE) provides research-based education, advocacy training, advocacy leadership and information to Canadians with arthritis. We help empower people living with all forms of arthritis to take control of their disease and to take action in healthcare and research decision making. ACE activities are guided by its members and led by people with arthritis, leading medical professionals and the ACE Advisory Board. To learn more about ACE, visit: www.jointhealth.org
Acknowledgements
Over the past 12 months, ACE received unrestricted grants-in-aid (financial and in-kind) from: AbbVie Corporation, Amgen Canada, Arthritis Research Canada, Canadian Institutes of Health Research, Celgene Inc., Eli Lilly Canada Inc., Hoffman-La Roche Limited, Innovative Medicines Canada, Janssen Inc., Merck Canada Inc., Novartis Pharmaceuticals Canada Inc., Pfizer Canada Inc., Sanofi Canada, St. Paul’s Hospital, UCB Canada Inc. and the University of British Columbia. ACE also receives unsolicited donations from its community members (people with arthritis) across Canada.
ACE’s information, programs and services and opinions are free from influence from individuals or organizations providing ACE unrestricted grant funding.
Disclaimer
The material contained on this website is provided for general information only. This website should not be relied on to suggest a course of treatment for a particular individual or as a substitute for consultation with qualified health professionals who are familiar with your individual medical needs. Should you have any healthcare related questions, you should contact your physician. You should never disregard medical advice or delay in seeking it because of something you have read on this or any website.
This site may provide links to other Internet sites only for the convenience of World Wide Web users. ACE is not responsible for the availability or content of these external sites, nor does ACE endorse, warrant or guarantee the products, services or information described or offered at these other Internet sites.
Although the information presented on this website is believed to be accurate at the time it is posted, this website could include inaccuracies, typographical errors or out-of-date information. This website may be changed at any time without prior notice.
