In this issue
- May is Ankylosing Spondylitis month
- What is Ankylosing Spondylitis?
- Q & A with Michael Mallinson
- Ask your Rheumatologist
- Arthritis Broadcast Network Ratings Soar in First Month of Launch
JointHealth™ insight Published May 2012
May is Ankylosing Spondylitis month
The arthritis spotlight shines on ankylosing spondylitis (AS) in May, marked by the Ankylosing Spondylitis International Federation designation of May 5th as World Ankylosing Spondylitis Day. Throughout the world, including Canada, patients, healthcare professionals and advocates in the international AS community take this day to stand up and be heard. In Canada, the Canadian Spondylitis Association (CSA), The Arthritis Society, and the Spondyloarthritis Research Consortium of Canada are hosting Patient Forums this year as part of the efforts to raise awareness and provide consumers the latest medical news and give an opportunity to have their questions answered during the expert panel sessions.
Arthritis Consumer Experts (ACE) has been a host and keen participant at past CSA forums, including being on the expert panel sessions where we have shared valuable information on biologic response modifier (“biologics”) coverage across Canada. ACE’s presentations informed AS patients about the importance of ensuring Canadians in all provinces have the same access to life saving treatments.
This year the Canadian Spondylitis Association Patient Forums occurred on May 12 in Toronto and is coming up on June 16 in Vancouver with a focus on the following key areas:
What is Ankylosing Spondylitis?
Ankylosing spondylitis is one of the most common types of chronic inflammatory arthritis. It affects the joints at the base of the spine where the spine joins the pelvis—the sacroiliac (SI) joints. Up to 1 in 200 people are estimated to have AS.
Ankylosing spondylitis can also affect the hips, knees, shoulders, and rib cage. The most common symptom of AS is long-term back pain, along with spinal stiffness in the morning or after a long period of rest (this is the main reason why AS is often misdiagnosed as ordinary “low back pain”).
A unique feature of AS is that, unlike many other forms of arthritis where women are most affected, three out of four people diagnosed with ankylosing spondylitis are men. Another characteristic of AS is that it tends to strike in the prime of life. Although it can occur at any age, it is most common in people between ages 15 and 40. Like other arthritis types, there is no known cure; however, it is treatable.
Q & A with Michael Mallinson,
President, Canadian Spondylitis Association

Q: Hi, Michael. Can you tell us about your organization?
A: The Canadian Spondylitis Association is a nonprofit national patient association formed in April 2006 to support and to advocate for those suffering from ankylosing spondylitis and associated spondyloarthritis diseases including psoriatic arthritis, enteropathic arthritis and reactive arthritis. Our goal is to be the leader in Canada providing support, education and advocacy for the spondyloarthritis patient community
Q: What are some misconceptions about ankylosing spondylitis?
A: Most people are unaware that AS strikes young people. The typical age of onset is between 17 and 35. Although people are aware that arthritis is a women’s disease, they are surprised when they found out AS has a significantly higher prevalence among men.
Q: What are the challenges in ankylosing spondylitis diagnosis?
A: AS is difficult to diagnose in the early stages. Because of this, AS is the most overlooked cause of persistent back pain in young adults. We are constantly educating people that it’s important to remember that signs of AS often may not be visible until the disease has progressed to a point where joint damage has already occurred. This is why the site of the stiffness, characteristics of onset of pain, and the time of day when pain is worst, may be the most important factors to analyze when diagnosing AS.
Q: How important is early detection?
A: It’s important for people to diagnose the cause of their pain and spinal stiffness. As in the case with most forms of inflammatory arthritis, early diagnosis and treatment of AS can be key factors in maintaining joint health and preventing disability and deformity. If the inflammation associated with AS continues unchecked, changes to the spinal column are likely to result, causing the spine to fuse solidly in a forward-stooped posture, spinal immobility and limitation of range of movement. If AS affects the hips, damage can result in the need for total hip replacement surgery.
Q: What impact does ankylosing spondylitis have on society and our economy?
A: Most people with spondylitis lead full and productive lives. Certain complications, however, can lead to absenteeism and disability. As one form of arthritis, it costs the North American economy billions of dollars in costs of care and productivity loss.
Ask your Rheumatologist
Significant advancements in medical treatments have occurred for AS during recent years and there are treatment options for those afflicted that can reduce the pain and symptoms of AS. When developing the ArthritisID and ArthritisID PRO apps, ACE spoke with rheumatologists at the Arthritis Research Centre of Canada (ARC) about treatment guidelines for the management of AS, including several groups of medications.
Q: What is the baseline medication treatment for AS?
A: Non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen (Advil® or Motrin IB®), naproxen (Naprosyn®), diclofenac (Voltaren®) are still the cornerstone of treatment and the first stage of medication in treating the pain and stiffness associated with spondylitis. However, NSAIDs can cause significant side effects, in particular, damage to the gastrointestinal tract. A different class of NSAIDs known as COX-2 inhibitors such as celecoxib (Celebrex®) reduce the risk of gastrointestinal complications associated with traditional NSAID therapy.
Q: What about cortisone treatment?
A: Glucocorticoid (sometimes called ‘cortisone’) is injected directly at the site of inflammation. Unlike other forms of arthritis, there is little evidence to support the use of glucocorticoid tablets such as prednisone or other “systemic corticosteroids” for disease involvement in the spine.
Q: When NSAIDs are not enough, patients may be prescribed a next stage of medications such as disease modifying anti-rheumatic drugs (DMARDS). What are your thoughts on these “second line medications?”
A: There is little evidence to support the use of traditional disease-modifying anti-rheumatic drugs (DMARDs) used in treating rheumatoid arthritis such as methotrexate, sulfasalazine, hydroxychloroquine, leflunomide and azathioprine for the treatment of spinal disease involvement. However, sulfasalazine may be used in patients with ankylosing spondylitis with peripheral (large joints such as elbows, wrists, knees, and ankles) disease involvement.
Q: What is your opinion on biologics, which studies have shown to be highly effective in treating not only the arthritis of the joints but the spinal arthritis associated with AS?
A: Anti-TNF biologic DMARDS (or “biologics”), specifically adalimumab (Humira®), etanercept (Enbrel®), golimumab (Simponi®), and infliximab (Remicade ®), have all been approved in Canada and shown great promise in treating AS—both the spinal inflammation and the peripheral inflammation.

Arthritis Broadcast Network Ratings Soar in First Month of Launch
The Arthritis Broadcast Network (ABN) has received an incredible first month of viewership across Canada and in the United States. This is just the beginning of a brand new experience for an arthritis audience of consumers and healthcare professionals to share some of their incredible life changing stories and work. The key to the sustainable success of the ABN is your involvement. How?
She lives with ankylosing spondylitis every day. Here, Nathalie tells us about her long fight with pain and frustration.

For Nathalie, it all started at the age of about 20 with uveitis wrongly diagnosed as a minor infection. In her thirties, she suffered from a kidney infection which could have had major consequences. In her late thirties, opiate type drugs, codeine and sleeping pills made up the cocktail that she would have to take every day to overcome the pain and her inability to sleep, except for a few hours, every night. Over the years, she had multiple visits to the hospital and consultations with general practitioners who unfortunately could not establish a proper diagnosis.
It was at the age of 41, after a long journey marked with pain, tiredness and frustrations, that she finally consulted a chiropractor who literally saved her life. Taking her seriously, he quickly made a diagnosis of AS and recommended that she consult a doctor to get a referral to see a rheumatologist. A diagnosis would soon be established with certainty and a treatment undertaken to finally improve her quality of life.
To get to know Nathalie a little better, we asked her a series of questions, to which she willingly answered. Here they are:
Q: How long ago were you diagnosed with AS?
A: It was 4 years ago. I was diagnosed at 41. I am now 45. After suffering for 21 years I finally got an answer. As funny as it seems, it was the happiest day of my life (after giving birth to my only daughter). I finally had proof I was not crazy and now had some options for treatment. IT GAVE ME HOPE!
Q: How long did it take to receive a diagnosis?
A: It took 21 years from the first symptom that was uveitis. But, I would say that I was searching for an answer for about 12 to 15 years, when the disease started to be more active and really disturb many parts of my life. The last 5 years before the diagnosis had been the hardest . . . Excruciating pain, no sleep and a feeling of hopelessness.
Q: What were your thoughts and feelings before you found out you had AS?
A: I was actually suicidal. I just could not cope with the excruciating pain anymore and the lack of sleep was making me so tired that I was in a major depression. I wrote a letter of goodbye for my daughter that I kept to remind me, at all times, that nothing in my life will probably be as bad or debilitating as the state I was before I got my diagnosis.
Q: What kind of treatment do you engage in? For example, what kinds of medication are you taking, have you changed your lifestyle, or have you sought alternative treatments?
A: I am now on Humira® (adalimumab), a biologic medication that is the only thing that has worked for me. I do need to rest more than the average person and avoid stress as much as I can. I eat well: lots of fresh stuff, almost nothing processed. I go to the chiropractor once in a while. I try to walk every day a bit with my dogs and I noticed that it helps a lot to stay active and exercise gently.
Q: Have you ever been hospitalized due to your AS?
A: I had a pyelonephritis around the age of 29, that was probably due to my immune system being over active. I was hospitalized then and in very bad shape. Both my kidneys were so inflamed that my blood was poisoned due to a high level of toxicity. I also had a surgery that I did not need for an infection on my leg that was really a pyoderma gangrenosum that was not diagnosed properly.
Q: How do you manage day-to-day life, work, or parenting? What strategies get you through the day?
A: I don’t work anymore and honestly as much as it was hard to accept at the beginning, I know now that it is for the best. I get to rest a lot more any time of the day when I feel sooooo tired that there is nothing left of energy inside of me. My daughter is now 18, but I can tell you that my disease impacted her life and my relationship with her in lots of ways. My strategies are really simple: as much rest as I need, good nutrition, walking with my dogs a bit every day, and trying to avoid stress. It is not perfect but I can say that at least I am able to go through day-to-day with more energy to do what needs to be done.
Q: Did receiving a diagnosis change the way you look at your life, friends, and family?
A: Yes I was now able to think that a treatment was available and that I will be able to go on living.
I HAD HOPE – finally.
Initially the diagnosis was a blessing, but than I had to learn to accept all what it will mean and also understand that I would have to give up a lot of things that I really cared about to be able to stay as healthy as I could. I had had a period of euphoria and afterwards a major depression. I tried to explain how I felt to my friends and family but I think only a sick person can truly understand the effects of a diseases on someone’s life. I don’t feel diminished at all because of it, but just extremely different from other people and it made it really hard to connect with others that are materialistic or shallow on the earlier state of my diagnosis. Now with the time that has passed I have more patience for people who worried about their grass or their broken nails . . . lol.
Q: What activities do you participate in that might surprise or inspire others who live with AS? For example, do you play a sport, mountain climb, or do creative work?
A: I still play golf . . . I love it . . . It is quite hard for me and I am really not too good at it, but I do it when I feel good and I don’t push myself too much. I have to accept that I have limitations and if I have pain maybe not playing for a hole or two. To get to relax is OK and at least I am still outside on a golf course in a beautiful surrounding, so instead of being mad at myself because I can’t play like the other golfer I try to think that I am very lucky to be there while having arthritis in almost every joint of my body. I also dance . . . I am taking lessons in ballroom dancing, cha cha, meringue, valse, tango, foxtrot, rumba and many others. It is a wonderful way to exercise while having fun and learning something new. I almost look sexy doing it with my arthritic body!
Nathalie writes in French about her experience of living with ankylosing spondylitis for the Arthritis Broadcast Network (ABN). Visit arthritisbroadcastnetwork.org to learn more about her, and discover the journey of a true fighter.

Coming soon: Next month, a new writer will be joining the ABN to tell us in English about living with AS.
We are always looking for more participation from arthritis consumers. If you would like to share your experience of living with this, or any other type(s) of arthritis, please submit your story to feedback@arthritisbroadcastnetwork.org.
Listening to you
We hope you find this information of use. Please tell us what you think by writing to us or emailing us at info@jointhealth.org. Through your ongoing and active participation, ACE can make its work more relevant to all Canadians living with arthritis.
Update your email or postal address
Please let us know of any changes by contacting ACE at info@jointhealth.org. This will ensure that you continue to receive your free email or print copy of JointHealth™ monthly.
Arthritis Consumer Experts (ACE)
Who We Are
Arthritis Consumer Experts (ACE) provides research-based education, advocacy training, advocacy leadership and information to Canadians with arthritis. We help empower people living with all forms of arthritis to take control of their disease and to take action in healthcare and research decision making. ACE activities are guided by its members and led by people with arthritis, leading medical professionals and the ACE Advisory Board. To learn more about ACE, visit: www.jointhealth.org
Acknowledgements
Over the past 12 months, ACE received unrestricted grants-in-aid from: Abbott Laboratories Ltd., Amgen Canada, Arthritis Research Centre of Canada, AstraZeneca Canada, Canadian Institutes of Health Research, GlaxoSmithKline, Hoffman-La Roche Canada Ltd., Merck & Co. Canada, Novartis Canada, Pfizer Canada, Sanofi-aventis Canada Inc., Takeda Canada, Inc., and UCB Canada Inc. ACE also receives unsolicited donations from its community members (people with arthritis) across Canada.
ACE thanks these private and public organizations and individuals.
Disclaimer
The material contained on this website is provided for general information only. This website should not be relied on to suggest a course of treatment for a particular individual or as a substitute for consultation with qualified health professionals who are familiar with your individual medical needs. Should you have any healthcare related questions, you should contact your physician. You should never disregard medical advice or delay in seeking it because of something you have read on this or any website.
This site may provide links to other Internet sites only for the convenience of World Wide Web users. ACE is not responsible for the availability or content of these external sites, nor does ACE endorse, warrant or guarantee the products, services or information described or offered at these other Internet sites.
Although the information presented on this website is believed to be accurate at the time it is posted, this website could include inaccuracies, typographical errors or out-of-date information. This website may be changed at any time without prior notice.
May is Ankylosing Spondylitis month
The arthritis spotlight shines on ankylosing spondylitis (AS) in May, marked by the Ankylosing Spondylitis International Federation designation of May 5th as World Ankylosing Spondylitis Day. Throughout the world, including Canada, patients, healthcare professionals and advocates in the international AS community take this day to stand up and be heard. In Canada, the Canadian Spondylitis Association (CSA), The Arthritis Society, and the Spondyloarthritis Research Consortium of Canada are hosting Patient Forums this year as part of the efforts to raise awareness and provide consumers the latest medical news and give an opportunity to have their questions answered during the expert panel sessions.
Arthritis Consumer Experts (ACE) has been a host and keen participant at past CSA forums, including being on the expert panel sessions where we have shared valuable information on biologic response modifier (“biologics”) coverage across Canada. ACE’s presentations informed AS patients about the importance of ensuring Canadians in all provinces have the same access to life saving treatments.
This year the Canadian Spondylitis Association Patient Forums occurred on May 12 in Toronto and is coming up on June 16 in Vancouver with a focus on the following key areas:
- Ankylosing Spondylitis (AS) and its treatment and management
- Psoriatic Arthritis (PsA) and its treatments
- Update on worldwide spondyloarthritis (SpA) research efforts
What is Ankylosing Spondylitis?
Ankylosing spondylitis is one of the most common types of chronic inflammatory arthritis. It affects the joints at the base of the spine where the spine joins the pelvis—the sacroiliac (SI) joints. Up to 1 in 200 people are estimated to have AS.
Ankylosing spondylitis can also affect the hips, knees, shoulders, and rib cage. The most common symptom of AS is long-term back pain, along with spinal stiffness in the morning or after a long period of rest (this is the main reason why AS is often misdiagnosed as ordinary “low back pain”).
A unique feature of AS is that, unlike many other forms of arthritis where women are most affected, three out of four people diagnosed with ankylosing spondylitis are men. Another characteristic of AS is that it tends to strike in the prime of life. Although it can occur at any age, it is most common in people between ages 15 and 40. Like other arthritis types, there is no known cure; however, it is treatable.
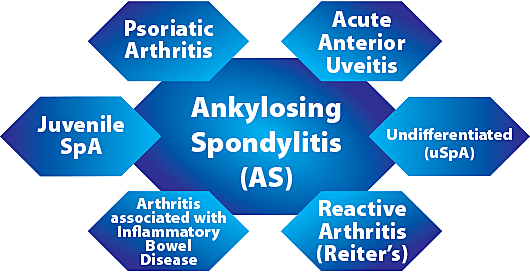
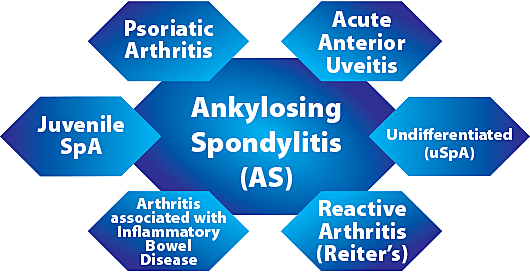
Spondyloarthritis is a group of diseases characterized by chronic inflammation of the pelvic joints and spine. Often, it is accompanied by arthritis in other joints. Spondyloarthritis affects at least the same number of Canadians as rheumatoid arthritis (1 in 100 people). Until recently, SpA was not well recognized and was under-researched in Canada. Ankylosing spondylitis and psoriatic arthritis fall under this group.
Q & A with Michael Mallinson,
President, Canadian Spondylitis Association

Q: Hi, Michael. Can you tell us about your organization?
A: The Canadian Spondylitis Association is a nonprofit national patient association formed in April 2006 to support and to advocate for those suffering from ankylosing spondylitis and associated spondyloarthritis diseases including psoriatic arthritis, enteropathic arthritis and reactive arthritis. Our goal is to be the leader in Canada providing support, education and advocacy for the spondyloarthritis patient community
Q: What are some misconceptions about ankylosing spondylitis?
A: Most people are unaware that AS strikes young people. The typical age of onset is between 17 and 35. Although people are aware that arthritis is a women’s disease, they are surprised when they found out AS has a significantly higher prevalence among men.
Q: What are the challenges in ankylosing spondylitis diagnosis?
A: AS is difficult to diagnose in the early stages. Because of this, AS is the most overlooked cause of persistent back pain in young adults. We are constantly educating people that it’s important to remember that signs of AS often may not be visible until the disease has progressed to a point where joint damage has already occurred. This is why the site of the stiffness, characteristics of onset of pain, and the time of day when pain is worst, may be the most important factors to analyze when diagnosing AS.
Q: How important is early detection?
A: It’s important for people to diagnose the cause of their pain and spinal stiffness. As in the case with most forms of inflammatory arthritis, early diagnosis and treatment of AS can be key factors in maintaining joint health and preventing disability and deformity. If the inflammation associated with AS continues unchecked, changes to the spinal column are likely to result, causing the spine to fuse solidly in a forward-stooped posture, spinal immobility and limitation of range of movement. If AS affects the hips, damage can result in the need for total hip replacement surgery.
Q: What impact does ankylosing spondylitis have on society and our economy?
A: Most people with spondylitis lead full and productive lives. Certain complications, however, can lead to absenteeism and disability. As one form of arthritis, it costs the North American economy billions of dollars in costs of care and productivity loss.
What’s the plan for treatment?
If your doctor believes you may have ankylosing spondylitis, you will usually be referred to a rheumatologist. Your rheumatologist will be the one to outline an effective treatment plan to help you manage the symptoms and minimize joint damage. AS treatment plans commonly involve pharmacological medication as well as essential non-pharmacological approaches. In particular, exercise and physical therapy, good posture practices and other treatments, such as applying heat and cold, are recommended to help maintain a range of motion and flexibility, relax muscles and reduce joint pain.
If your doctor believes you may have ankylosing spondylitis, you will usually be referred to a rheumatologist. Your rheumatologist will be the one to outline an effective treatment plan to help you manage the symptoms and minimize joint damage. AS treatment plans commonly involve pharmacological medication as well as essential non-pharmacological approaches. In particular, exercise and physical therapy, good posture practices and other treatments, such as applying heat and cold, are recommended to help maintain a range of motion and flexibility, relax muscles and reduce joint pain.
Ask your Rheumatologist
Significant advancements in medical treatments have occurred for AS during recent years and there are treatment options for those afflicted that can reduce the pain and symptoms of AS. When developing the ArthritisID and ArthritisID PRO apps, ACE spoke with rheumatologists at the Arthritis Research Centre of Canada (ARC) about treatment guidelines for the management of AS, including several groups of medications.
Q: What is the baseline medication treatment for AS?
A: Non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen (Advil® or Motrin IB®), naproxen (Naprosyn®), diclofenac (Voltaren®) are still the cornerstone of treatment and the first stage of medication in treating the pain and stiffness associated with spondylitis. However, NSAIDs can cause significant side effects, in particular, damage to the gastrointestinal tract. A different class of NSAIDs known as COX-2 inhibitors such as celecoxib (Celebrex®) reduce the risk of gastrointestinal complications associated with traditional NSAID therapy.
Q: What about cortisone treatment?
A: Glucocorticoid (sometimes called ‘cortisone’) is injected directly at the site of inflammation. Unlike other forms of arthritis, there is little evidence to support the use of glucocorticoid tablets such as prednisone or other “systemic corticosteroids” for disease involvement in the spine.
Q: When NSAIDs are not enough, patients may be prescribed a next stage of medications such as disease modifying anti-rheumatic drugs (DMARDS). What are your thoughts on these “second line medications?”
A: There is little evidence to support the use of traditional disease-modifying anti-rheumatic drugs (DMARDs) used in treating rheumatoid arthritis such as methotrexate, sulfasalazine, hydroxychloroquine, leflunomide and azathioprine for the treatment of spinal disease involvement. However, sulfasalazine may be used in patients with ankylosing spondylitis with peripheral (large joints such as elbows, wrists, knees, and ankles) disease involvement.
Q: What is your opinion on biologics, which studies have shown to be highly effective in treating not only the arthritis of the joints but the spinal arthritis associated with AS?
A: Anti-TNF biologic DMARDS (or “biologics”), specifically adalimumab (Humira®), etanercept (Enbrel®), golimumab (Simponi®), and infliximab (Remicade ®), have all been approved in Canada and shown great promise in treating AS—both the spinal inflammation and the peripheral inflammation.

Arthritis Broadcast Network Ratings Soar in First Month of Launch
The Arthritis Broadcast Network (ABN) has received an incredible first month of viewership across Canada and in the United States. This is just the beginning of a brand new experience for an arthritis audience of consumers and healthcare professionals to share some of their incredible life changing stories and work. The key to the sustainable success of the ABN is your involvement. How?
- View ABN programs at arthritisbroadcastnetwork.org and join the thousands of others in the ABN community
- Become an ABN Insider to receive news and feature stories from ABN
- Send your comments, personal story, photos, videos, Facebook post, tweet, e-mail to feedback@arthritisbroadcastnetwork.org
Visit www.jointhealth.org or download the apps developed by the Arthritis is cured! (if you want it) National Arthritis Awareness Program (NAAP), ArthritisID and ArthritisID PRO to learn more about ankylosing spondylitis and find helpful resources. The NAAP is a collaborative effort of Arthritis Consumer Experts (ACE) and the Arthritis Research Centre of Canada (ARC).

She lives with ankylosing spondylitis every day. Here, Nathalie tells us about her long fight with pain and frustration.

For Nathalie, it all started at the age of about 20 with uveitis wrongly diagnosed as a minor infection. In her thirties, she suffered from a kidney infection which could have had major consequences. In her late thirties, opiate type drugs, codeine and sleeping pills made up the cocktail that she would have to take every day to overcome the pain and her inability to sleep, except for a few hours, every night. Over the years, she had multiple visits to the hospital and consultations with general practitioners who unfortunately could not establish a proper diagnosis.
It was at the age of 41, after a long journey marked with pain, tiredness and frustrations, that she finally consulted a chiropractor who literally saved her life. Taking her seriously, he quickly made a diagnosis of AS and recommended that she consult a doctor to get a referral to see a rheumatologist. A diagnosis would soon be established with certainty and a treatment undertaken to finally improve her quality of life.
To get to know Nathalie a little better, we asked her a series of questions, to which she willingly answered. Here they are:
Q: How long ago were you diagnosed with AS?
A: It was 4 years ago. I was diagnosed at 41. I am now 45. After suffering for 21 years I finally got an answer. As funny as it seems, it was the happiest day of my life (after giving birth to my only daughter). I finally had proof I was not crazy and now had some options for treatment. IT GAVE ME HOPE!
Q: How long did it take to receive a diagnosis?
A: It took 21 years from the first symptom that was uveitis. But, I would say that I was searching for an answer for about 12 to 15 years, when the disease started to be more active and really disturb many parts of my life. The last 5 years before the diagnosis had been the hardest . . . Excruciating pain, no sleep and a feeling of hopelessness.
Q: What were your thoughts and feelings before you found out you had AS?
A: I was actually suicidal. I just could not cope with the excruciating pain anymore and the lack of sleep was making me so tired that I was in a major depression. I wrote a letter of goodbye for my daughter that I kept to remind me, at all times, that nothing in my life will probably be as bad or debilitating as the state I was before I got my diagnosis.
Q: What kind of treatment do you engage in? For example, what kinds of medication are you taking, have you changed your lifestyle, or have you sought alternative treatments?
A: I am now on Humira® (adalimumab), a biologic medication that is the only thing that has worked for me. I do need to rest more than the average person and avoid stress as much as I can. I eat well: lots of fresh stuff, almost nothing processed. I go to the chiropractor once in a while. I try to walk every day a bit with my dogs and I noticed that it helps a lot to stay active and exercise gently.
Q: Have you ever been hospitalized due to your AS?
A: I had a pyelonephritis around the age of 29, that was probably due to my immune system being over active. I was hospitalized then and in very bad shape. Both my kidneys were so inflamed that my blood was poisoned due to a high level of toxicity. I also had a surgery that I did not need for an infection on my leg that was really a pyoderma gangrenosum that was not diagnosed properly.
Q: How do you manage day-to-day life, work, or parenting? What strategies get you through the day?
A: I don’t work anymore and honestly as much as it was hard to accept at the beginning, I know now that it is for the best. I get to rest a lot more any time of the day when I feel sooooo tired that there is nothing left of energy inside of me. My daughter is now 18, but I can tell you that my disease impacted her life and my relationship with her in lots of ways. My strategies are really simple: as much rest as I need, good nutrition, walking with my dogs a bit every day, and trying to avoid stress. It is not perfect but I can say that at least I am able to go through day-to-day with more energy to do what needs to be done.
Q: Did receiving a diagnosis change the way you look at your life, friends, and family?
A: Yes I was now able to think that a treatment was available and that I will be able to go on living.
I HAD HOPE – finally.
Initially the diagnosis was a blessing, but than I had to learn to accept all what it will mean and also understand that I would have to give up a lot of things that I really cared about to be able to stay as healthy as I could. I had had a period of euphoria and afterwards a major depression. I tried to explain how I felt to my friends and family but I think only a sick person can truly understand the effects of a diseases on someone’s life. I don’t feel diminished at all because of it, but just extremely different from other people and it made it really hard to connect with others that are materialistic or shallow on the earlier state of my diagnosis. Now with the time that has passed I have more patience for people who worried about their grass or their broken nails . . . lol.
Q: What activities do you participate in that might surprise or inspire others who live with AS? For example, do you play a sport, mountain climb, or do creative work?
A: I still play golf . . . I love it . . . It is quite hard for me and I am really not too good at it, but I do it when I feel good and I don’t push myself too much. I have to accept that I have limitations and if I have pain maybe not playing for a hole or two. To get to relax is OK and at least I am still outside on a golf course in a beautiful surrounding, so instead of being mad at myself because I can’t play like the other golfer I try to think that I am very lucky to be there while having arthritis in almost every joint of my body. I also dance . . . I am taking lessons in ballroom dancing, cha cha, meringue, valse, tango, foxtrot, rumba and many others. It is a wonderful way to exercise while having fun and learning something new. I almost look sexy doing it with my arthritic body!
Nathalie writes in French about her experience of living with ankylosing spondylitis for the Arthritis Broadcast Network (ABN). Visit arthritisbroadcastnetwork.org to learn more about her, and discover the journey of a true fighter.

Coming soon: Next month, a new writer will be joining the ABN to tell us in English about living with AS.
We are always looking for more participation from arthritis consumers. If you would like to share your experience of living with this, or any other type(s) of arthritis, please submit your story to feedback@arthritisbroadcastnetwork.org.
Listening to you
We hope you find this information of use. Please tell us what you think by writing to us or emailing us at info@jointhealth.org. Through your ongoing and active participation, ACE can make its work more relevant to all Canadians living with arthritis.
Update your email or postal address
Please let us know of any changes by contacting ACE at info@jointhealth.org. This will ensure that you continue to receive your free email or print copy of JointHealth™ monthly.
Arthritis Consumer Experts (ACE)
Who We Are
Arthritis Consumer Experts (ACE) provides research-based education, advocacy training, advocacy leadership and information to Canadians with arthritis. We help empower people living with all forms of arthritis to take control of their disease and to take action in healthcare and research decision making. ACE activities are guided by its members and led by people with arthritis, leading medical professionals and the ACE Advisory Board. To learn more about ACE, visit: www.jointhealth.org
Acknowledgements
Over the past 12 months, ACE received unrestricted grants-in-aid from: Abbott Laboratories Ltd., Amgen Canada, Arthritis Research Centre of Canada, AstraZeneca Canada, Canadian Institutes of Health Research, GlaxoSmithKline, Hoffman-La Roche Canada Ltd., Merck & Co. Canada, Novartis Canada, Pfizer Canada, Sanofi-aventis Canada Inc., Takeda Canada, Inc., and UCB Canada Inc. ACE also receives unsolicited donations from its community members (people with arthritis) across Canada.
ACE thanks these private and public organizations and individuals.
Disclaimer
The material contained on this website is provided for general information only. This website should not be relied on to suggest a course of treatment for a particular individual or as a substitute for consultation with qualified health professionals who are familiar with your individual medical needs. Should you have any healthcare related questions, you should contact your physician. You should never disregard medical advice or delay in seeking it because of something you have read on this or any website.
This site may provide links to other Internet sites only for the convenience of World Wide Web users. ACE is not responsible for the availability or content of these external sites, nor does ACE endorse, warrant or guarantee the products, services or information described or offered at these other Internet sites.
Although the information presented on this website is believed to be accurate at the time it is posted, this website could include inaccuracies, typographical errors or out-of-date information. This website may be changed at any time without prior notice.
