In this issue
- What is osteoarthritis?
- Sport injury and osteoarthritis
- Diagnosis of osteoarthritis
- Treating and managing osteoarthritis
- Lifestyle changes
- Equity considerations for osteoarthritis care
- Joint replacement surgery
JointHealth™ insight Published December 2022


Listening to you
We hope you find this information of use. Please tell us what you think by writing to us or emailing us at feedback@jointhealth.org. Through your ongoing and active participation, ACE can make its work more relevant to all Canadians living with arthritis.
Update your email or postal address
Please let us know of any changes by contacting ACE at feedback@jointhealth.org. This will ensure that you continue to receive your free email or print copy of JointHealth™ insight.
Arthritis Consumer Experts (ACE)
Who We Are
Arthritis Consumer Experts (ACE) and its team members acknowledge that they gather and work on the traditional, ancestral and unceded territory of the Coast Salish peoples -ʷməθkʷəy̓əm (Musqueam), Sḵwx̱wú7mesh (Squamish), and Səl̓ílwətaʔ/Selilwitulh (Tsleil-Waututh) Nations.
Arthritis Consumer Experts (ACE) operates as a non-profit and provides free research based education and information to Canadians with arthritis. We help (em)power people living with all forms of arthritis to take control of their disease and to take action in healthcare and research decision making. ACE activities are guided by its members and led by people with arthritis, scientific and medical experts on the ACE Advisory Board. To learn more about ACE, visit www.jointhealth.org
Disclosures
Over the past 12 months, ACE received grants-in-aid from: Arthritis Research Canada, Amgen Canada, Canadian Biosimilars Forum, Canadian Institutes of Health Research, Canadian Rheumatology Association, Eli Lilly Canada, Fresenius Kabi Canada, Novartis Canada, Organon Canada, Pfizer Canada, Sandoz Canada, Teva Canada, UCB Canada, and the University of British Columbia.
ACE also received unsolicited donations from its community members (people with arthritis) across Canada.
ACE thanks funders for their support to help the nearly 6 million Canadians living with osteoarthritis, rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis and the many other forms of the disease.
Disclaimer
The material contained on this website is provided for general information only. This website should not be relied on to suggest a course of treatment for a particular individual or as a substitute for consultation with qualified health professionals who are familiar with your individual medical needs. Should you have any healthcare related questions, you should contact your physician. You should never disregard medical advice or delay in seeking it because of something you have read on this or any website.
This site may provide links to other Internet sites only for the convenience of World Wide Web users. ACE is not responsible for the availability or content of these external sites, nor does ACE endorse, warrant or guarantee the products, services or information described or offered at these other Internet sites.
Although the information presented on this website is believed to be accurate at the time it is posted, this website could include inaccuracies, typographical errors or out-of-date information. This website may be changed at any time without prior notice.


Osteoarthritis (OA) is a degenerative joint disease that is the most common type of arthritis and a major cause of difficulties with mobility and disability globally:
 In the past, OA was often dismissed as the inevitable “wear and tear” of the joints. People were told to “just live” with the pain as they got older. In this issue of JointHealth™ insight, we debunk that myth and take a closer look at how people can address joint pain and OA symptoms early on through education, lifestyle changes, and different treatments in order to live a full life with OA.
In the past, OA was often dismissed as the inevitable “wear and tear” of the joints. People were told to “just live” with the pain as they got older. In this issue of JointHealth™ insight, we debunk that myth and take a closer look at how people can address joint pain and OA symptoms early on through education, lifestyle changes, and different treatments in order to live a full life with OA.
What is OA?
Osteoarthritis is caused by the breakdown in cartilage in the joints. Cartilage is a protein substance that acts as a cushion between bones, allowing joints to glide smoothly. Without it, bones can start to rub against each other, and movements can become stiff and unpleasant. Unlike other forms of arthritis, osteoarthritis is a non-inflammatory condition. This means that it is not an autoimmune condition. However, it is progressive meaning symptoms may get worse, which may lead to inflammation, if the underlying cause is not addressed. OA—particularly knee OA—is one of the fastest growing chronic diseases worldwide, due to an increase in sedentary lifestyle, knee injury and lifespan. What is the cost of OA to the healthcare system?
What is the cost of OA to the healthcare system?
OA is a leading cause of chronic pain and loss of mobility in Canada and is associated with reduced productivity and increased use of health care resources. It is estimated that by 2040, 12 million Canadians will have OA.2
Researchers from the Alberta Bone and Joint Health Institute estimate the rising rates of OA will cost the Canadian economy:
Dr. Sharif, an Alberta Bone and Joint Health Institute post-doctoral fellow based at the University of Calgary, states: “Our findings underscore the importance of implementing public strategies to prevent OA while also developing ways to maintain the workplace productivity of people who have the disease. Canada could lose a significant portion of its shrinking work force to osteoarthritis unless policies are developed now to sustain the employability of people who have pain and loss of function in their hips and knees.”
Who can develop osteoarthritis?
Osteoarthritis is by far the most common type of arthritis affecting approximately five million Canadians adults. Risk factors for osteoarthritis include age, a family history of the disease, excess body weight that increases the pressure on joints, as well as joint injury. The greatest increase in OA is seen among young people (20-59 years), due largely to childhood obesity, knee injury and repeated stress on a joint. Unlike some other forms of arthritis where women are most affected, women and men are equally likely to be affected by OA. It strikes most commonly after the age of 45, but people of all ages are at risk.4 What is the connection between sport injury and OA?
What is the connection between sport injury and OA?
One of the most important risk factors for knee OA is a joint injury. In Canada, approximately 500,000 youth hurt their knee while participating in sports annually. Half will go on to develop OA within 10 years. Dr. Jackie Whittaker is a Research Scientist of Musculoskeletal Rehabilitation at Arthritis Research Canada. The focus of her research is understanding the connection between youth sport knee injuries and early onset osteoarthritis, as well as osteoarthritis prevention. Whittaker, who is also a physiotherapist, created a unique, online knee health program called SOAR, or Stop OsteoARthritis, to help people boost their recovery from a knee injury and reduce their risk of developing OA. The program involves education, personalized exercise, activity tracking and weekly action planning.
“One of the biggest myths about osteoarthritis is that nothing can be done to prevent it,” said Dr. Jackie Whittaker, a research scientist at Arthritis Research Canada. “We have really good evidence to suggest that many things can be done to minimize a person’s pain and improve their function to reduce symptoms and prevent osteoarthritis from impeding everyday life.”
Currently, the treatment of young athletes that suffer a knee injury focuses on returning them to sport. Few seek care beyond their injury, and little effort is made to prevent OA. Dr. Whittaker wants to change that by focussing her research on what someone can do after an injury to minimize their risk for developing OA.
“My research is focused on trying to reduce risk factors for osteoarthritis after a youth sport knee injury. I want to increase awareness in young people who hurt their knees playing sports. I want them to know they are at risk for developing OA, but also that they can take steps to prevent it. We have identified that obesity and muscle weakness are risk factors. So, keeping muscles strong and staying active after an injury to avoid weight gain are important. The red flag isn’t when you have swelling and pain. It’s when you are becoming less and less active because of your knee. The last thing you want someone to do is stop sport or physical activities altogether. However, it can be challenging and sometimes support is needed,” said Dr. Whittaker.
The SOAR 8-week Digital Knee Health Program for people at risk of OA includes: Getting a diagnosis of osteoarthritis
Getting a diagnosis of osteoarthritis
The most common symptoms are joint pain and discomfort. Osteoarthritis can affect any joint. Hands and weight-bearing joints—including the spine, hips and knees—are most often affected.
As is the case with most forms of arthritis, early diagnosis of osteoarthritis can be a key factor in maintaining joint health and preventing disability and deformity. There are things you can do to slow the progression of joint damage and reduce the potential for future disability. Getting a diagnosis is the crucial first step in an osteoarthritis treatment plan.
Osteoarthritis tool for patients
Good communication between patients and their health care providers is very important in reaching an accurate diagnosis and building effective treatment plans. Based on that evidence, Arthritis Consumer Experts, other patient organizations, as well as scientific and clinical experts in OA, have developed the Talk to Your Doctor About Joint Pain Handout designed to improve the quality of life for individuals with arthritis, including their physical activity, sleep, mental health (like mood or depression), relationships and work life, specifically by: How to treat and manage OA
How to treat and manage OA
According to one of Canada’s leading OA experts, Dr. Gillian Hawker, Rheumatologist and Professor of Medicine, University of Toronto: “Although effective therapies exist, the high prevalence of other medical conditions in people with OA makes management challenging. As many as 90 per cent of people with OA have at least one additional chronic condition—most often diabetes, heart disease, and high blood pressure.”
Currently, there are no medications that effectively treat the underlying disease process of osteoarthritis, only medications to treat the symptoms associated with the disease such as pain. For this reason, lifestyle changes and physical activity are often considered the “best medicines” to treat osteoarthritis.
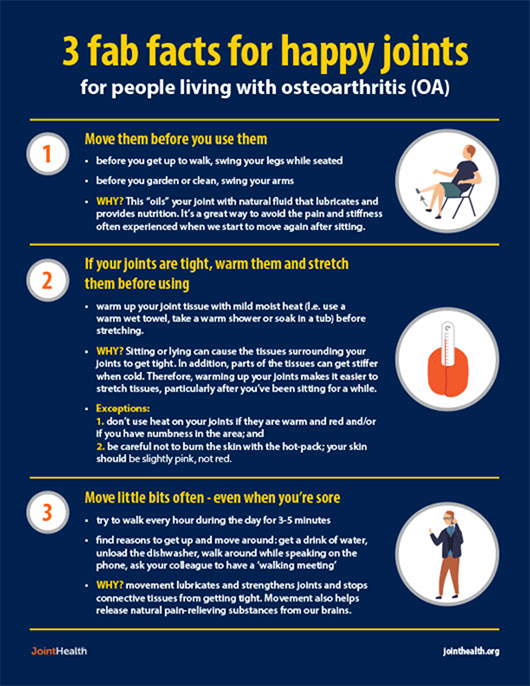
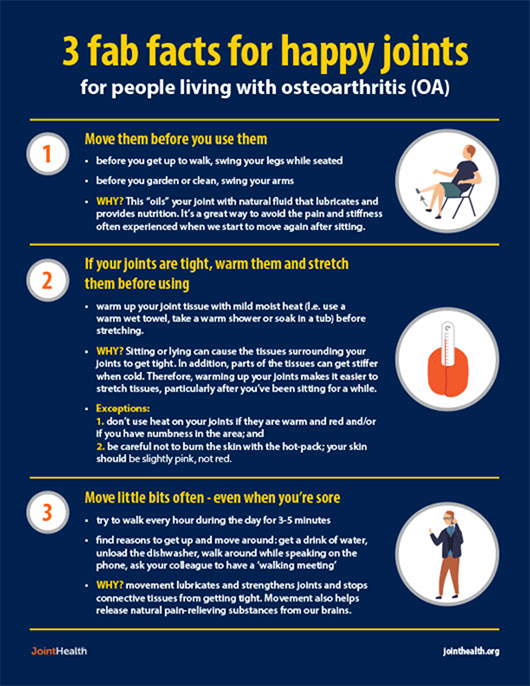
Lifestyle changes
An important part of managing your osteoarthritis is to maintain a healthy body weight, which could reduce the load placed on joints, and in many cases, minimize pain. People with osteoarthritis, like everyone, should aim to achieve 150 minutes of physical activity each week. A well-balanced diet can also play a huge role to support our metabolic health. Physical Activity
Physical Activity
Physical activity is another important component of the OA treatment plan as movement signals joints to produce more cartilage, which combats OA. The key is to participate in the right kinds of activities. Generally, activities that put less stress on joints, like swimming and other water-based types of activities, are an ideal start. Once joints are strengthened, patients can slowly transition to an elliptical or a stationary bicycle for greater cardiovascular challenge and begin to incorporate mobility exercises.5 Lastly, there is good evidence to suggest that strength training can help to build muscles around the joint, increase flexibility and reduce pain.
 Equity considerations for non-surgical osteoarthritis care
Equity considerations for non-surgical osteoarthritis care
Osteoarthritis care is an unmet health need for many diverse individuals living in Canada. Historical injustice, institutionalize medicine, and the socioeconomic divide have resulted in health disparities amongst hard to reach groups. For example, research suggests that people living in rural settings, those experiencing low income or unemployment, and Indigenous Peoples, have an increased risk for OA and have more severe symptoms (Lin et al. (2017)6. In Canada, Cheryl Barnabe has led a team of researchers to look at the inequitable care received by Indigenous Peoples living in Alberta (Barnabe et al. (2015).7 More resources must be invested to address these disparities.
Elizabeth Houlding, a physiotherapy student from the University of Toronto, has published research on equity considerations for osteoarthritis care.8 For her project, she approached osteoarthritis health care providers and asked them to rate the different non-surgical interventions such as physical activity and assistive devices using an equity lens. Specifically, she examined the feasibility, health system effects, universality and impact on inequities for each intervention. In a recent #ArthritisAtHome, Ms. Houlding spoke about her findings from her work and how they are being used to move knowledge into practice.
Medication for OA
Before starting on a medication therapy, it is important to have a throughout conversation with your health care provider about possible side effects and complications with your current medications. In mild to moderate cases of osteoarthritis, joint pain may be sufficiently treated with an over-the-counter pain reliever, like acetaminophen (Tylenol®). Acetaminophen can be effective in reducing pain but is not an anti-inflammatory medication and cannot stop joint damage.
If a pain reliever like acetaminophen is not enough, doctors may prescribe a non-steroidal anti-inflammatory drug (NSAID). Examples of NSAIDs available without a prescription include ibuprofen (Motrin® or Advil®) and acetylsalicylic acid (Aspirin®). More powerful NSAIDs require a prescription. These include naproxen (Naprosyn®). These are potent medications which may reduce joint inflammation and pain, but do not work to reduce joint damage. In rare cases, NSAIDs have been linked to cause serious cardiovascular, kidney or gastro-intestinal side effects, like stomach ulcers.9 COX-2 inhibitors are a type of NSAID that work to reduce inflammation but do not carry the same risk of gastrointestinal side effects.
Sometimes, an injection of corticosteroid (sometimes called 'cortisone') into the affected joint may help to reduce the inflammation of advanced osteoarthritis in the hip and knee. Cortisone injections can help in situations where mobility is impacted or pain is severe.10 For some people, medication therapies may help in the short term; while others may respond well and get a longer lasting benefit. What is a joint replacement?
What is a joint replacement?
The most common type of joint surgery for osteoarthritis is joint replacement; knees and hips are the most common joints to be treated. If first-line treatment options like education, physical activity and weight management as well as medication are not enough to manage your osteoarthritis pain and problems with day-to-day function, your doctor may refer you to a surgeon to see if surgery is the right option for you.
In total, 55,285 knee replacements were performed in Canada between 2020 and 2021. And over $1.3 billion was spent on hip and knee replacement surgeries during that time.11 The number of hip and knee replacements has increased each year over the past 10 years, except for 2020-2021, when many surgeries were cancelled due to the COVID-19 pandemic. Learn more about joint replacement
Learn more about joint replacement
ACE looked at joint replacement for arthritis in a special JointHealth™ insight, with a focus on the time before surgery, including information about what a joint replacement is, decision making for surgery, bilateral knee replacements and preparing for surgery. In a follow up JointHealth™ insight, ACE discussed recovering from joint replacement surgery, where we feature a patient’s perspective on the recovery and rehabilitation process.
Key OA Takeaways
Osteoarthritis is so much more than a “wear and tear” condition. A combination of factors play a role in the development of osteoarthritis, such as:
References
`
- OA affects young and old adults
- Approximately 5% of Canadians between 35 and 54 years of age have OA
- Approximately 30% of Canadians between 50 and 70 years of age have problems such as poor sleep, fatigue, depressed mood and loss of independence related to OA1
- 80% of people with OA have knee OA and many of these individuals injured their joint earlier in life
 In the past, OA was often dismissed as the inevitable “wear and tear” of the joints. People were told to “just live” with the pain as they got older. In this issue of JointHealth™ insight, we debunk that myth and take a closer look at how people can address joint pain and OA symptoms early on through education, lifestyle changes, and different treatments in order to live a full life with OA.
In the past, OA was often dismissed as the inevitable “wear and tear” of the joints. People were told to “just live” with the pain as they got older. In this issue of JointHealth™ insight, we debunk that myth and take a closer look at how people can address joint pain and OA symptoms early on through education, lifestyle changes, and different treatments in order to live a full life with OA.What is OA?
Osteoarthritis is caused by the breakdown in cartilage in the joints. Cartilage is a protein substance that acts as a cushion between bones, allowing joints to glide smoothly. Without it, bones can start to rub against each other, and movements can become stiff and unpleasant. Unlike other forms of arthritis, osteoarthritis is a non-inflammatory condition. This means that it is not an autoimmune condition. However, it is progressive meaning symptoms may get worse, which may lead to inflammation, if the underlying cause is not addressed. OA—particularly knee OA—is one of the fastest growing chronic diseases worldwide, due to an increase in sedentary lifestyle, knee injury and lifespan.
 What is the cost of OA to the healthcare system?
What is the cost of OA to the healthcare system?OA is a leading cause of chronic pain and loss of mobility in Canada and is associated with reduced productivity and increased use of health care resources. It is estimated that by 2040, 12 million Canadians will have OA.2
Researchers from the Alberta Bone and Joint Health Institute estimate the rising rates of OA will cost the Canadian economy:
- an estimated $17.5 billion a year in lost productivity by 2031 due to OA symptoms; and,
- a greater number of people will be forced to stop working or work less due to mobility limitations and pain.3
Dr. Sharif, an Alberta Bone and Joint Health Institute post-doctoral fellow based at the University of Calgary, states: “Our findings underscore the importance of implementing public strategies to prevent OA while also developing ways to maintain the workplace productivity of people who have the disease. Canada could lose a significant portion of its shrinking work force to osteoarthritis unless policies are developed now to sustain the employability of people who have pain and loss of function in their hips and knees.”
Who can develop osteoarthritis?
Osteoarthritis is by far the most common type of arthritis affecting approximately five million Canadians adults. Risk factors for osteoarthritis include age, a family history of the disease, excess body weight that increases the pressure on joints, as well as joint injury. The greatest increase in OA is seen among young people (20-59 years), due largely to childhood obesity, knee injury and repeated stress on a joint. Unlike some other forms of arthritis where women are most affected, women and men are equally likely to be affected by OA. It strikes most commonly after the age of 45, but people of all ages are at risk.4
 What is the connection between sport injury and OA?
What is the connection between sport injury and OA?One of the most important risk factors for knee OA is a joint injury. In Canada, approximately 500,000 youth hurt their knee while participating in sports annually. Half will go on to develop OA within 10 years. Dr. Jackie Whittaker is a Research Scientist of Musculoskeletal Rehabilitation at Arthritis Research Canada. The focus of her research is understanding the connection between youth sport knee injuries and early onset osteoarthritis, as well as osteoarthritis prevention. Whittaker, who is also a physiotherapist, created a unique, online knee health program called SOAR, or Stop OsteoARthritis, to help people boost their recovery from a knee injury and reduce their risk of developing OA. The program involves education, personalized exercise, activity tracking and weekly action planning.
“One of the biggest myths about osteoarthritis is that nothing can be done to prevent it,” said Dr. Jackie Whittaker, a research scientist at Arthritis Research Canada. “We have really good evidence to suggest that many things can be done to minimize a person’s pain and improve their function to reduce symptoms and prevent osteoarthritis from impeding everyday life.”
Currently, the treatment of young athletes that suffer a knee injury focuses on returning them to sport. Few seek care beyond their injury, and little effort is made to prevent OA. Dr. Whittaker wants to change that by focussing her research on what someone can do after an injury to minimize their risk for developing OA.
“My research is focused on trying to reduce risk factors for osteoarthritis after a youth sport knee injury. I want to increase awareness in young people who hurt their knees playing sports. I want them to know they are at risk for developing OA, but also that they can take steps to prevent it. We have identified that obesity and muscle weakness are risk factors. So, keeping muscles strong and staying active after an injury to avoid weight gain are important. The red flag isn’t when you have swelling and pain. It’s when you are becoming less and less active because of your knee. The last thing you want someone to do is stop sport or physical activities altogether. However, it can be challenging and sometimes support is needed,” said Dr. Whittaker.
The SOAR 8-week Digital Knee Health Program for people at risk of OA includes:
- One day knee camp
- 8-week exercise and physical activity
- Weekly one-on-one physiotherapy counselling
- Monitor patients’ knee and act early when they notice inactivity
- Feed patient’s cartilage through daily weight bearing exercises
- Build the patient’s muscle through strength training
- Control the patient’s weight (odds of obesity increase 2.5 times after a knee injury) through weekly moderate-vigorous aerobic activity and a healthy diet
 Getting a diagnosis of osteoarthritis
Getting a diagnosis of osteoarthritisThe most common symptoms are joint pain and discomfort. Osteoarthritis can affect any joint. Hands and weight-bearing joints—including the spine, hips and knees—are most often affected.
- Joint pain and/or stiffness lasting for more than two weeks
- Swelling in joints of the hands and feet
- Reduced muscle strength and joint mobility
As is the case with most forms of arthritis, early diagnosis of osteoarthritis can be a key factor in maintaining joint health and preventing disability and deformity. There are things you can do to slow the progression of joint damage and reduce the potential for future disability. Getting a diagnosis is the crucial first step in an osteoarthritis treatment plan.
Osteoarthritis tool for patients
Good communication between patients and their health care providers is very important in reaching an accurate diagnosis and building effective treatment plans. Based on that evidence, Arthritis Consumer Experts, other patient organizations, as well as scientific and clinical experts in OA, have developed the Talk to Your Doctor About Joint Pain Handout designed to improve the quality of life for individuals with arthritis, including their physical activity, sleep, mental health (like mood or depression), relationships and work life, specifically by:
- Assisting those with or at risk of OA, in having better conversations with their doctors or other health care professionals, by informing them about the care they can expect to receive.
- Helping patients identify the causes of their joint pain and loss of mobility.
- Informing them of the basics of primary prevention strategies and self-care methods.
 How to treat and manage OA
How to treat and manage OAAccording to one of Canada’s leading OA experts, Dr. Gillian Hawker, Rheumatologist and Professor of Medicine, University of Toronto: “Although effective therapies exist, the high prevalence of other medical conditions in people with OA makes management challenging. As many as 90 per cent of people with OA have at least one additional chronic condition—most often diabetes, heart disease, and high blood pressure.”
Currently, there are no medications that effectively treat the underlying disease process of osteoarthritis, only medications to treat the symptoms associated with the disease such as pain. For this reason, lifestyle changes and physical activity are often considered the “best medicines” to treat osteoarthritis.
Lifestyle changes
An important part of managing your osteoarthritis is to maintain a healthy body weight, which could reduce the load placed on joints, and in many cases, minimize pain. People with osteoarthritis, like everyone, should aim to achieve 150 minutes of physical activity each week. A well-balanced diet can also play a huge role to support our metabolic health.
 Physical Activity
Physical ActivityPhysical activity is another important component of the OA treatment plan as movement signals joints to produce more cartilage, which combats OA. The key is to participate in the right kinds of activities. Generally, activities that put less stress on joints, like swimming and other water-based types of activities, are an ideal start. Once joints are strengthened, patients can slowly transition to an elliptical or a stationary bicycle for greater cardiovascular challenge and begin to incorporate mobility exercises.5 Lastly, there is good evidence to suggest that strength training can help to build muscles around the joint, increase flexibility and reduce pain.
|
We’re GLA:D™ you asked Canada’s aging baby boomers are much more active than previous generations. Keeping active is imperative for good general health and healthy aging. Often, joint pain is a barrier to stay active, which is understandable, people get anxious and as a result stop being active to ease the pain. According to Dr. Ewa Roos, co-developer of the GLA:D™ program in Denmark, an education and exercise program for those with stiff or painful knees or hips or with knee or hip osteoarthritis, this is the wrong thing to do as research shows supervised exercise reduces pain up to 30%: “Contemporary OA treatment therefore starts with patient education and exercise. People with knee or hip pain who have participated in education and 12 sessions of neuromuscular exercise experience reduced sick leave, reduced intake of analgesics, reduced pain, improved physical function and walking speed, and increased physical activity.” Based on the success of the program in Denmark, the GLA:D™ education and exercise program for knee and hip OA is now being made available in Canada. |
| Fact or Fiction? | ||
|
OA is inevitable Young people get OA too I must be in a lot of pain before getting help Weight bearing activities help my knee OA It is harder to lose weight than prevent weight gain |
Fiction Fact Fiction Fact Fact |
|
 Equity considerations for non-surgical osteoarthritis care
Equity considerations for non-surgical osteoarthritis careOsteoarthritis care is an unmet health need for many diverse individuals living in Canada. Historical injustice, institutionalize medicine, and the socioeconomic divide have resulted in health disparities amongst hard to reach groups. For example, research suggests that people living in rural settings, those experiencing low income or unemployment, and Indigenous Peoples, have an increased risk for OA and have more severe symptoms (Lin et al. (2017)6. In Canada, Cheryl Barnabe has led a team of researchers to look at the inequitable care received by Indigenous Peoples living in Alberta (Barnabe et al. (2015).7 More resources must be invested to address these disparities.
Elizabeth Houlding, a physiotherapy student from the University of Toronto, has published research on equity considerations for osteoarthritis care.8 For her project, she approached osteoarthritis health care providers and asked them to rate the different non-surgical interventions such as physical activity and assistive devices using an equity lens. Specifically, she examined the feasibility, health system effects, universality and impact on inequities for each intervention. In a recent #ArthritisAtHome, Ms. Houlding spoke about her findings from her work and how they are being used to move knowledge into practice.
| We acknowledge diverse values and beliefs around treatment. Your health care provider will be able to discuss and recommend personalized treatments that may differ from the information provided in this issue. If you have questions about the topics in this issue, please email them to feedback@jointhealth.org |
Before starting on a medication therapy, it is important to have a throughout conversation with your health care provider about possible side effects and complications with your current medications. In mild to moderate cases of osteoarthritis, joint pain may be sufficiently treated with an over-the-counter pain reliever, like acetaminophen (Tylenol®). Acetaminophen can be effective in reducing pain but is not an anti-inflammatory medication and cannot stop joint damage.
If a pain reliever like acetaminophen is not enough, doctors may prescribe a non-steroidal anti-inflammatory drug (NSAID). Examples of NSAIDs available without a prescription include ibuprofen (Motrin® or Advil®) and acetylsalicylic acid (Aspirin®). More powerful NSAIDs require a prescription. These include naproxen (Naprosyn®). These are potent medications which may reduce joint inflammation and pain, but do not work to reduce joint damage. In rare cases, NSAIDs have been linked to cause serious cardiovascular, kidney or gastro-intestinal side effects, like stomach ulcers.9 COX-2 inhibitors are a type of NSAID that work to reduce inflammation but do not carry the same risk of gastrointestinal side effects.
Sometimes, an injection of corticosteroid (sometimes called 'cortisone') into the affected joint may help to reduce the inflammation of advanced osteoarthritis in the hip and knee. Cortisone injections can help in situations where mobility is impacted or pain is severe.10 For some people, medication therapies may help in the short term; while others may respond well and get a longer lasting benefit.
 What is a joint replacement?
What is a joint replacement?The most common type of joint surgery for osteoarthritis is joint replacement; knees and hips are the most common joints to be treated. If first-line treatment options like education, physical activity and weight management as well as medication are not enough to manage your osteoarthritis pain and problems with day-to-day function, your doctor may refer you to a surgeon to see if surgery is the right option for you.
In total, 55,285 knee replacements were performed in Canada between 2020 and 2021. And over $1.3 billion was spent on hip and knee replacement surgeries during that time.11 The number of hip and knee replacements has increased each year over the past 10 years, except for 2020-2021, when many surgeries were cancelled due to the COVID-19 pandemic.
 Learn more about joint replacement
Learn more about joint replacementACE looked at joint replacement for arthritis in a special JointHealth™ insight, with a focus on the time before surgery, including information about what a joint replacement is, decision making for surgery, bilateral knee replacements and preparing for surgery. In a follow up JointHealth™ insight, ACE discussed recovering from joint replacement surgery, where we feature a patient’s perspective on the recovery and rehabilitation process.
Key OA Takeaways
Osteoarthritis is so much more than a “wear and tear” condition. A combination of factors play a role in the development of osteoarthritis, such as:
- Receiving proper care and rehabilitation after a joint injury
- Maintaining a healthy body weight to body mass index
- Consulting a health care professional to determine if medication or surgical treatments may be required
References
| 1 | Bone and Joint Canada: Osteoarthritis https://boneandjointcanada.com/osteoarthritis/ |
| 2 | Arthritis Research Canada. https://www.arthritisresearch.ca/knee-osteoarthrtis-nonsurgical-options/ |
| 3 | Alberta Bone and Joint Health Institute: News Release. https://www.albertaboneandjoint.com/archive/osteoarthritis-productivity-loss-canada-arthritis-society-arthritis-alliance-canada/ |
| 4 | Zhang & Jordan (2010). Epidemiology of osteoarthritis. https://doi.org/10.1016/j.cger.2010.03.001 |
| 5 | Exercise is Medicine website: Exercising with Osteoarthritis. https://www.exerciseismedicine.org/assets/page_documents/steoarthritis.pdf |
| 6 | Lin et al. (2017). Unmet Needs of Aboriginal Australians With Musculoskeletal Pain: A Mixed-Method Systematic Review. https://doi.org/10.1002/acr.23493 |
| 7 | Barnabe et al. (2015). Imbalance of prevalence and specialty care for osteoarthritis for first nations people in Alberta, Canada. https://doi.org/10.3899/jrheum.140551 |
| 8 | Experts prioritize osteoarthritis non-surgical interventions from Cochrane systemic reviews for translation into “Evidence4Equity” summaries. 2021 https://link.springer.com/article/10.1186/s12939-021-01477-4 |
| 9 | Cryer, B., & Mahaffey, K. W. (2014). Gastrointestinal ulcers, role of aspirin, and clinical outcomes: pathobiology, diagnosis, and treatment. Journal of multidisciplinary healthcare, 7, 137–146. https://doi.org/10.2147/JMDH.S54324 |
| 10 | Zeng et al. 2019. Intra-articular corticosteroids and the risk of knee osteoarthritis progression: results from the Osteoarthritis Initiative. https://doi.org/10.1016/j.joca.2019.01.007 |
| 11 | Canadian Institute for Health Information: Hip and Knee Replacements in Canada. September 2022. https://www.cihi.ca/en/cjrr-annual-report-hip-and-knee-replacements-in-canada |
Listening to you
We hope you find this information of use. Please tell us what you think by writing to us or emailing us at feedback@jointhealth.org. Through your ongoing and active participation, ACE can make its work more relevant to all Canadians living with arthritis.
Update your email or postal address
Please let us know of any changes by contacting ACE at feedback@jointhealth.org. This will ensure that you continue to receive your free email or print copy of JointHealth™ insight.
Arthritis Consumer Experts (ACE)
Who We Are
Arthritis Consumer Experts (ACE) and its team members acknowledge that they gather and work on the traditional, ancestral and unceded territory of the Coast Salish peoples -ʷməθkʷəy̓əm (Musqueam), Sḵwx̱wú7mesh (Squamish), and Səl̓ílwətaʔ/Selilwitulh (Tsleil-Waututh) Nations.
Arthritis Consumer Experts (ACE) operates as a non-profit and provides free research based education and information to Canadians with arthritis. We help (em)power people living with all forms of arthritis to take control of their disease and to take action in healthcare and research decision making. ACE activities are guided by its members and led by people with arthritis, scientific and medical experts on the ACE Advisory Board. To learn more about ACE, visit www.jointhealth.org
Disclosures
Over the past 12 months, ACE received grants-in-aid from: Arthritis Research Canada, Amgen Canada, Canadian Biosimilars Forum, Canadian Institutes of Health Research, Canadian Rheumatology Association, Eli Lilly Canada, Fresenius Kabi Canada, Novartis Canada, Organon Canada, Pfizer Canada, Sandoz Canada, Teva Canada, UCB Canada, and the University of British Columbia.
ACE also received unsolicited donations from its community members (people with arthritis) across Canada.
ACE thanks funders for their support to help the nearly 6 million Canadians living with osteoarthritis, rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis and the many other forms of the disease.
Disclaimer
The material contained on this website is provided for general information only. This website should not be relied on to suggest a course of treatment for a particular individual or as a substitute for consultation with qualified health professionals who are familiar with your individual medical needs. Should you have any healthcare related questions, you should contact your physician. You should never disregard medical advice or delay in seeking it because of something you have read on this or any website.
This site may provide links to other Internet sites only for the convenience of World Wide Web users. ACE is not responsible for the availability or content of these external sites, nor does ACE endorse, warrant or guarantee the products, services or information described or offered at these other Internet sites.
Although the information presented on this website is believed to be accurate at the time it is posted, this website could include inaccuracies, typographical errors or out-of-date information. This website may be changed at any time without prior notice.
