In this issue
- What is Lupus?
- What causes Lupus?
- Who is affected by Lupus?
- What lupus research tells us
- ACE National Survey on Virtual Care Services for People Living Arthritis: The experiences of lupus patients
- Lupus care & treatment
- Lupus resources
JointHealth™ insight Published February 2022


Listening to you
We hope you find this information of use. Please tell us what you think by writing to us or emailing us at feedback@jointhealth.org. Through your ongoing and active participation, ACE can make its work more relevant to all Canadians living with arthritis.
Update your email or postal address
Please let us know of any changes by contacting ACE at feedback@jointhealth.org. This will ensure that you continue to receive your free email or print copy of JointHealth™ insight.
Arthritis Consumer Experts (ACE)
Who We Are
Arthritis Consumer Experts (ACE) and its team members acknowledge that they gather and work on the traditional, ancestral and unceded territory of the Coast Salish peoples -ʷməθkʷəy̓əm (Musqueam), Sḵwx̱wú7mesh (Squamish), and Səl̓ílwətaʔ/Selilwitulh (Tsleil-Waututh) Nations.
Arthritis Consumer Experts (ACE) operates as a non-profit and provides free research based education and information to Canadians with arthritis. We help (em)power people living with all forms of arthritis to take control of their disease and to take action in healthcare and research decision making. ACE activities are guided by its members and led by people with arthritis, scientific and medical experts on the ACE Advisory Board. To learn more about ACE, visit www.jointhealth.org
Disclosures
Over the past 12 months, ACE received grants-in-aid from: Amgen Canada, Arthritis Research Canada, Canadian Biosimilars Forum, Canadian Rheumatology Association, Eli Lilly Canada, Fresenius Kabi Canada, Merck Canada, Novartis Canada, Organon Canada, Pfizer Canada, Sandoz Canada, Teva Canada, UCB Canada and the University of British Columbia.
ACE also received unsolicited donations from its community members (people with arthritis) across Canada.
ACE thanks funders for their support to help the nearly 6 million Canadians living with osteoarthritis, rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis and the many other forms of the disease.
Disclaimer
The material contained on this website is provided for general information only. This website should not be relied on to suggest a course of treatment for a particular individual or as a substitute for consultation with qualified health professionals who are familiar with your individual medical needs. Should you have any healthcare related questions, you should contact your physician. You should never disregard medical advice or delay in seeking it because of something you have read on this or any website.
This site may provide links to other Internet sites only for the convenience of World Wide Web users. ACE is not responsible for the availability or content of these external sites, nor does ACE endorse, warrant or guarantee the products, services or information described or offered at these other Internet sites.
Although the information presented on this website is believed to be accurate at the time it is posted, this website could include inaccuracies, typographical errors or out-of-date information. This website may be changed at any time without prior notice.


What is Lupus?
Lupus is an unpredictable disease in which a person’s immune system produces an excess of proteins called antibodies that attach themselves to various structures in the body. The accumulation of these antibodies in the tissues can cause inflammation, damage and pain. The most common form of lupus is systemic lupus erythematosus (SLE). Approximately 15,000 Canadians are affected by SLE. Lupus symptoms and severity vary from patient to patient, for some, lupus is life-threatening and for others, it’s entirely manageable.
What causes Lupus?
 Despite many years of research, the cause of lupus is still not known. Scientists believe there are several things that may trigger the formation of the antibodies, including genetic, hormonal and environmental factors. Some of the possible triggers include:
Despite many years of research, the cause of lupus is still not known. Scientists believe there are several things that may trigger the formation of the antibodies, including genetic, hormonal and environmental factors. Some of the possible triggers include:
 Who is affected by Lupus?
Who is affected by Lupus?
Although lupus can affect anybody, 90% of lupus patients are women. Of these, 90% develop the condition during their reproductive years.
Health effects
Additional problems that come with lupus include: What lupus research tells us
What lupus research tells us
Researchers at Arthritis Research Canada (ARC) are some of the world’s leading authorities on lupus. A 2022 ARC study revealed that the risk of premature death in SLE patients compared to the general population has not improved in recent years. Lupus is associated with significant premature mortality caused by kidney disease, infections and cardiovascular disease.
ARC scientists examined two time periods, 1997-2005 and 2006-2014, and observed a 95 per cent and 74 per cent increased risk of overall deaths due to SLE relative to the general population in each time period, respectively.
“Mortality rates for systemic lupus erythematosus patients are not improving over time and this is concerning,” said Dr. Antonio Aviña-Zubieta, a rheumatologist and senior scientist at Arthritis Research Canada. “Previous research showed improvements in mortality from the 1970s to 2000s, but these recent findings highlight a need for further interventions in managing this disease.”
Dr. Aviña-Zubieta added that such interventions could include the development of new therapeutic agents, strategies for earlier disease detection and more comprehensive measures in the management of serious, life-threatening complications.
A second ARC study from 2021 found one in five patients with SLE develop severe infections with 21 per cent of those infections causing death. This is the first study to evaluate the risk of severe infections in a large group of SLE patients from the general population.
“Our research found that SLE is associated with an 82 per cent increased risk of severe infection when compared to non-SLE and a 61 per cent increased risk of infection-related mortality,” said Kai Zhao, a research trainee at Arthritis Research Canada. “These are important findings because they show that infections are one of the leading causes of premature death in patients living with this disease.”
The increased risk of infection is thought to be a result of two factors. First, immune system dysfunctions caused by SLE. Second, use of immunosuppressive medications and glucocorticoids. These medications inhibit the immune network and, therefore, decrease resistance to a wide variety of bacterial, viral, and fungal agents.
ACE National Survey on Virtual Care Services for People Living Arthritis: The experiences of lupus patients
In November 2021, Arthritis Consumer Experts (ACE) presented findings from its patient-led survey on virtual care at the American College of Rheumatology’s annual meeting. During this presentation, ACE encouraged feedback from community members who attended the conference as well as those who were following along through social media. People living with lupus told us that they were interested in learning about disease-specific findings. They wanted to see how people living with lupus answered the survey and what these findings could uncover about the specific virtual care experiences and preferences of the lupus community.
 Who were lupus survey respondents?
Who were lupus survey respondents?
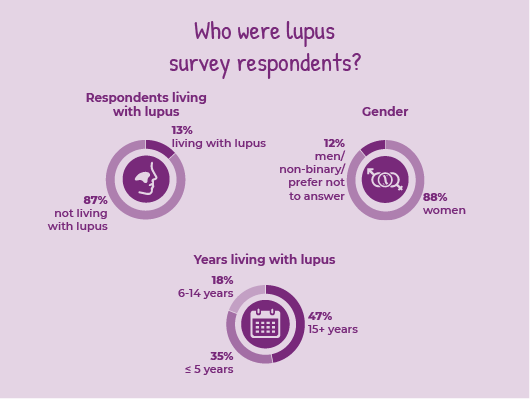
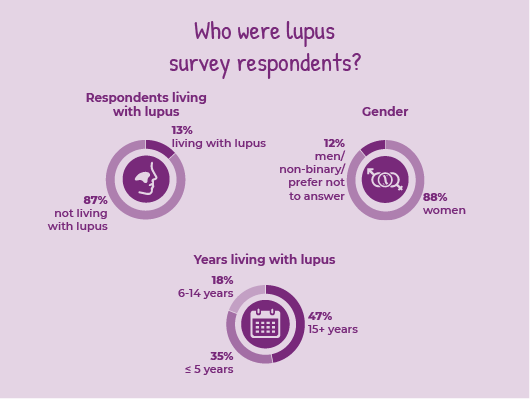
Just over 13% of all survey respondents (34 people) reported that they were living with lupus.
Over 88% of lupus survey respondents were women. Nearly half (47%) had been living with the disease for over 15 years, while 35% were living with lupus for 5 years or less.
Virtual care use before and during the COVID-19 pandemic
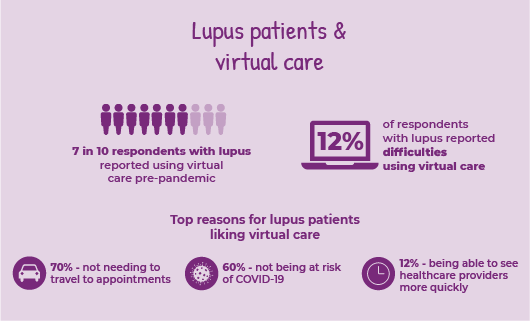
Many people with lupus who took our survey (71%) were already using some form of virtual care (VC) prior to March 2020. The number of lupus patients using VC rose to 88% during the pandemic.
As part of the survey, ACE asked respondents if any factors have made it difficult to use virtual care services. While most people with lupus said they had no issues, 12% reported difficulties of some kind. Difficulties included cost of electronics, access to the internet, lack of translation services and feeling uncomfortable using the VC technology offered by healthcare providers.
How did virtual care use for people with lupus differ from general survey respondents?
When compared to all survey respondents, a higher proportion of respondents with lupus were already using VC pre-pandemic (59% of all respondents vs. 71% of lupus respondents).
A smaller proportion of people with lupus reported difficulties using VC in comparison to all survey respondents (16% of all respondents vs. 12% of those with lupus experienced difficulties).
 Lupus patient satisfaction with virtual care
Lupus patient satisfaction with virtual care
Overall, respondents with lupus were generally satisfied sharing health concerns and getting advice through virtual care.
The most common reasons for liking virtual healthcare services were:
Respondents with lupus reported a slightly higher satisfaction rate for VC services in comparison to general respondents (85% of all respondents vs. 90% of lupus respondents were very satisfied, satisfied or somewhat satisfied with their VC experiences). In comparison to all survey respondents, a greater proportion of people with lupus liked the convenience factor of in-person meetings with allied healthcare providers, i.e., meeting providers at the same time/in the same place (selected by 29% of all respondents vs. 50% of lupus respondents).
Lupus patient preferences for the future of virtual care
Like general survey respondents, a majority of those with lupus wanted a mix of in-person and virtual care services in the future. Lupus respondents were most interested in continuing to have a VC option for appointments with their rheumatologist (wanted by 62% of lupus respondents) and their family doctor (59%).
Overall, 71% of people living with lupus who took the survey felt it was at least somewhat important to have continued access to virtual care services after the COVID-19 pandemic is over.
How did preferences on the future of virtual care for people with lupus differ from general survey respondents?
In comparison to all respondents, there is a smaller proportion of people with lupus who said it was very important to have continued access to virtual care services (30% of all respondents vs. 21% of respondents with lupus). However, in comparison to all respondents, those with lupus have a greater interest in specifically seeing their rheumatologists virtually post-pandemic (49% of all respondents want the option to see their rheumatologist virtually vs 62% of lupus respondents).
 Lupus care & treatment
Lupus care & treatment
Living and coping with lupus can be challenging. The physical symptoms of lupus can be severe and debilitating, especially during disease episodes or flares. These physical symptoms can also have a powerful impact on other aspects of a patient’s life, including their mental and emotional wellbeing, relationships with family and friends, and their employment.
The best way for people to keep lupus under control is by following their treatment plan and practicing positive self-care. These steps can help: Lupus resources
Lupus resources
To learn more about living with lupus, including lifestyle tips and treatment information, check out the following resources:
Lupus is an unpredictable disease in which a person’s immune system produces an excess of proteins called antibodies that attach themselves to various structures in the body. The accumulation of these antibodies in the tissues can cause inflammation, damage and pain. The most common form of lupus is systemic lupus erythematosus (SLE). Approximately 15,000 Canadians are affected by SLE. Lupus symptoms and severity vary from patient to patient, for some, lupus is life-threatening and for others, it’s entirely manageable.
What causes Lupus?
 Despite many years of research, the cause of lupus is still not known. Scientists believe there are several things that may trigger the formation of the antibodies, including genetic, hormonal and environmental factors. Some of the possible triggers include:
Despite many years of research, the cause of lupus is still not known. Scientists believe there are several things that may trigger the formation of the antibodies, including genetic, hormonal and environmental factors. Some of the possible triggers include:
- Hormones (females between the age of 15 and 45 are most commonly affected)
- Certain medications
- Dietary factors
- Viruses and bacteria
- Stress
- Genetics
- Pregnancy
- Exposure to UV light
 Who is affected by Lupus?
Who is affected by Lupus?Although lupus can affect anybody, 90% of lupus patients are women. Of these, 90% develop the condition during their reproductive years.
Health effects
Additional problems that come with lupus include:
- Inflammation of the kidney, which occurs in up to 60% of adults with lupus (and two-thirds of children). It can cause high blood pressure, blood in the urine, frothy urine and swelling of the legs
- Raynaud’s disease which causes fingers and/or toes to turn white or blue when cold
- Sjögren’s syndrome which causes dry eyes, mouth
- Swelling in feet, hands or around eyes
- Hair loss that can be caused by lupus itself or medications used to treat it
- Blood problems including anemia (low red blood cell count), low platelet count, low white blood cell count and blood clots
- Memory problems or confusion
 What lupus research tells us
What lupus research tells usResearchers at Arthritis Research Canada (ARC) are some of the world’s leading authorities on lupus. A 2022 ARC study revealed that the risk of premature death in SLE patients compared to the general population has not improved in recent years. Lupus is associated with significant premature mortality caused by kidney disease, infections and cardiovascular disease.
ARC scientists examined two time periods, 1997-2005 and 2006-2014, and observed a 95 per cent and 74 per cent increased risk of overall deaths due to SLE relative to the general population in each time period, respectively.
“Mortality rates for systemic lupus erythematosus patients are not improving over time and this is concerning,” said Dr. Antonio Aviña-Zubieta, a rheumatologist and senior scientist at Arthritis Research Canada. “Previous research showed improvements in mortality from the 1970s to 2000s, but these recent findings highlight a need for further interventions in managing this disease.”
Dr. Aviña-Zubieta added that such interventions could include the development of new therapeutic agents, strategies for earlier disease detection and more comprehensive measures in the management of serious, life-threatening complications.
A second ARC study from 2021 found one in five patients with SLE develop severe infections with 21 per cent of those infections causing death. This is the first study to evaluate the risk of severe infections in a large group of SLE patients from the general population.
“Our research found that SLE is associated with an 82 per cent increased risk of severe infection when compared to non-SLE and a 61 per cent increased risk of infection-related mortality,” said Kai Zhao, a research trainee at Arthritis Research Canada. “These are important findings because they show that infections are one of the leading causes of premature death in patients living with this disease.”
The increased risk of infection is thought to be a result of two factors. First, immune system dysfunctions caused by SLE. Second, use of immunosuppressive medications and glucocorticoids. These medications inhibit the immune network and, therefore, decrease resistance to a wide variety of bacterial, viral, and fungal agents.
ACE National Survey on Virtual Care Services for People Living Arthritis: The experiences of lupus patients
In November 2021, Arthritis Consumer Experts (ACE) presented findings from its patient-led survey on virtual care at the American College of Rheumatology’s annual meeting. During this presentation, ACE encouraged feedback from community members who attended the conference as well as those who were following along through social media. People living with lupus told us that they were interested in learning about disease-specific findings. They wanted to see how people living with lupus answered the survey and what these findings could uncover about the specific virtual care experiences and preferences of the lupus community.
 Who were lupus survey respondents?
Who were lupus survey respondents?Just over 13% of all survey respondents (34 people) reported that they were living with lupus.
Over 88% of lupus survey respondents were women. Nearly half (47%) had been living with the disease for over 15 years, while 35% were living with lupus for 5 years or less.
Virtual care use before and during the COVID-19 pandemic
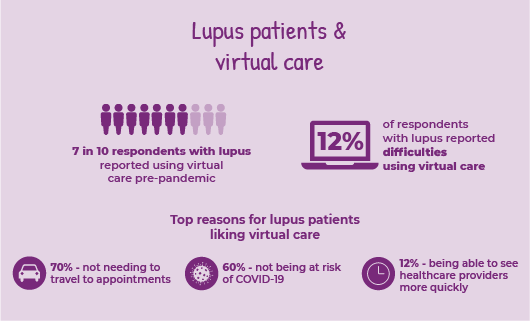
Many people with lupus who took our survey (71%) were already using some form of virtual care (VC) prior to March 2020. The number of lupus patients using VC rose to 88% during the pandemic.
As part of the survey, ACE asked respondents if any factors have made it difficult to use virtual care services. While most people with lupus said they had no issues, 12% reported difficulties of some kind. Difficulties included cost of electronics, access to the internet, lack of translation services and feeling uncomfortable using the VC technology offered by healthcare providers.
How did virtual care use for people with lupus differ from general survey respondents?
When compared to all survey respondents, a higher proportion of respondents with lupus were already using VC pre-pandemic (59% of all respondents vs. 71% of lupus respondents).
A smaller proportion of people with lupus reported difficulties using VC in comparison to all survey respondents (16% of all respondents vs. 12% of those with lupus experienced difficulties).
 Lupus patient satisfaction with virtual care
Lupus patient satisfaction with virtual careOverall, respondents with lupus were generally satisfied sharing health concerns and getting advice through virtual care.
The most common reasons for liking virtual healthcare services were:
- Not needing to travel to appointments, liked by nearly 70% of lupus respondents.
- Not being at risk of COVID-19, liked by 60% of lupus respondents. Twelve percent (12%) of people with lupus also liked that they saw healthcare providers more quickly than usual with VC.
Respondents with lupus reported a slightly higher satisfaction rate for VC services in comparison to general respondents (85% of all respondents vs. 90% of lupus respondents were very satisfied, satisfied or somewhat satisfied with their VC experiences). In comparison to all survey respondents, a greater proportion of people with lupus liked the convenience factor of in-person meetings with allied healthcare providers, i.e., meeting providers at the same time/in the same place (selected by 29% of all respondents vs. 50% of lupus respondents).
Lupus patient preferences for the future of virtual care
Like general survey respondents, a majority of those with lupus wanted a mix of in-person and virtual care services in the future. Lupus respondents were most interested in continuing to have a VC option for appointments with their rheumatologist (wanted by 62% of lupus respondents) and their family doctor (59%).
Overall, 71% of people living with lupus who took the survey felt it was at least somewhat important to have continued access to virtual care services after the COVID-19 pandemic is over.
How did preferences on the future of virtual care for people with lupus differ from general survey respondents?
In comparison to all respondents, there is a smaller proportion of people with lupus who said it was very important to have continued access to virtual care services (30% of all respondents vs. 21% of respondents with lupus). However, in comparison to all respondents, those with lupus have a greater interest in specifically seeing their rheumatologists virtually post-pandemic (49% of all respondents want the option to see their rheumatologist virtually vs 62% of lupus respondents).
 Lupus care & treatment
Lupus care & treatmentLiving and coping with lupus can be challenging. The physical symptoms of lupus can be severe and debilitating, especially during disease episodes or flares. These physical symptoms can also have a powerful impact on other aspects of a patient’s life, including their mental and emotional wellbeing, relationships with family and friends, and their employment.
The best way for people to keep lupus under control is by following their treatment plan and practicing positive self-care. These steps can help:
- Learn how to tell that a flare is coming
- See your doctors regularly
- Reduce stress by setting realistic goals for yourself
- Limit the time you spend in the sun and in fluorescent and halogen light
- Choose healthy foods most of the time
- Get enough sleep and rest
- Exercise moderately with your doctor’s OK and when you’re feeling up to it
- Anticoagulants to help prevent blood clots
- Anti-inflammatories to help with pain and inflammation
- Antimalarials to protect skin from rashes and UV light
- Biologics to help your immune system work correctly
- Immunosuppressives to help keep your immune system from attacking your body
- Steroids to help with inflammation
 Lupus resources
Lupus resourcesTo learn more about living with lupus, including lifestyle tips and treatment information, check out the following resources:
Listening to you
We hope you find this information of use. Please tell us what you think by writing to us or emailing us at feedback@jointhealth.org. Through your ongoing and active participation, ACE can make its work more relevant to all Canadians living with arthritis.
Update your email or postal address
Please let us know of any changes by contacting ACE at feedback@jointhealth.org. This will ensure that you continue to receive your free email or print copy of JointHealth™ insight.
Arthritis Consumer Experts (ACE)
Who We Are
Arthritis Consumer Experts (ACE) and its team members acknowledge that they gather and work on the traditional, ancestral and unceded territory of the Coast Salish peoples -ʷməθkʷəy̓əm (Musqueam), Sḵwx̱wú7mesh (Squamish), and Səl̓ílwətaʔ/Selilwitulh (Tsleil-Waututh) Nations.
Arthritis Consumer Experts (ACE) operates as a non-profit and provides free research based education and information to Canadians with arthritis. We help (em)power people living with all forms of arthritis to take control of their disease and to take action in healthcare and research decision making. ACE activities are guided by its members and led by people with arthritis, scientific and medical experts on the ACE Advisory Board. To learn more about ACE, visit www.jointhealth.org
Disclosures
Over the past 12 months, ACE received grants-in-aid from: Amgen Canada, Arthritis Research Canada, Canadian Biosimilars Forum, Canadian Rheumatology Association, Eli Lilly Canada, Fresenius Kabi Canada, Merck Canada, Novartis Canada, Organon Canada, Pfizer Canada, Sandoz Canada, Teva Canada, UCB Canada and the University of British Columbia.
ACE also received unsolicited donations from its community members (people with arthritis) across Canada.
ACE thanks funders for their support to help the nearly 6 million Canadians living with osteoarthritis, rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis and the many other forms of the disease.
Disclaimer
The material contained on this website is provided for general information only. This website should not be relied on to suggest a course of treatment for a particular individual or as a substitute for consultation with qualified health professionals who are familiar with your individual medical needs. Should you have any healthcare related questions, you should contact your physician. You should never disregard medical advice or delay in seeking it because of something you have read on this or any website.
This site may provide links to other Internet sites only for the convenience of World Wide Web users. ACE is not responsible for the availability or content of these external sites, nor does ACE endorse, warrant or guarantee the products, services or information described or offered at these other Internet sites.
Although the information presented on this website is believed to be accurate at the time it is posted, this website could include inaccuracies, typographical errors or out-of-date information. This website may be changed at any time without prior notice.
