In this issue
- Aging and arthritis
- Age and other risk factors for arthritis
- Looking at gender
- Genetics
- Yes, you can: Taking control of your arthritis
- Diet and nutrition
- Exercise as medicine
- No smoking, please
- Getting social, avoiding isolation
- Sleepless in arthritis
- Tips for better sleep
- Get involved in sleep research
JointHealth™ insight Published December 2021


 In a 2021 national survey, Arthritis Consumer Experts (ACE) attempted to identify inequities and gaps in arthritis self-advocacy – who is experiencing them and what some of the challenges are in advocating for the best arthritis care possible. One of the key insights that many respondents shared was a desire to learn more about aging and arthritis.
In a 2021 national survey, Arthritis Consumer Experts (ACE) attempted to identify inequities and gaps in arthritis self-advocacy – who is experiencing them and what some of the challenges are in advocating for the best arthritis care possible. One of the key insights that many respondents shared was a desire to learn more about aging and arthritis.
In this issue of JointHealth™ insight, we look at the complex relationship between aging and arthritis.
It’s one of the biggest misconceptions about arthritis. Most people believe that arthritis is an old person’s disease and that it is entirely a consequence of aging. If that were the case, arthritis would be inevitable — and it’s not.
There are more than 100 different types of arthritis, a disease that affects people of all ages, from babies to older adults; in fact, more than three in five people diagnosed with arthritis are under the age of 65.
One of the reasons people assume arthritis is an inevitable consequence of aging is that the risk of developing the most common type of arthritis, osteoarthritis, increases with age. The risk of developing osteoporosis, a condition often confused with osteoarthritis, also increases with age. While the risk of developing osteoarthritis increases with age, keep in mind that it is not the only contributing factor: Age and other risk factors for arthritis
Age and other risk factors for arthritis
Let’s now look at aging and other risk factors for arthritis and ways to prevent and live your best with arthritis.
Aging with arthritis
With aging of the population, the number of older adults evaluated in rheumatology clinics is expected to increase dramatically in Canada and the rest of the world. Age is a primary risk factor for most types of arthritis, and increases as you get older. For example, as the population ages, osteoarthritis (OA) becomes more common. Your weight is the biggest modifiable risk factor for developing OA as excess weight places additional stress on weight-bearing joints in your hip and knee.
Researchers have also identified numerous contributing factors for “elderly onset” of inflammatory arthritis, including smoking, periodontitis, and viral infections. There may also be an association with menopause and hormonal changes.
Older arthritis patients are at higher risk than younger patients for falls and decline in the ability to perform daily physical activities such as holding a cup, lifting a grocery bag, or walking to a car. This emphasizes the importance of early diagnosis and treatment for older arthritis patients to prevent these complications.
At the 2021 American College of Rheumatology annual scientific conference, researchers shared presentations at a Scientific Study session – “Multicomplexity in the Aging Patient with Rheumatoid Arthritis” - on how to improve the models of care for older patients. These researchers stressed how important it is for rheumatologists and arthritis health professionals to be aware of issues such as multimorbidity (patient with two or more chronic diseases) and polypharmacy (the use of multiple medicines that is common in older patient populations with multimorbidities) that pose unique challenges and barriers to outcomes for older patients.
For example, arthritis can make it harder for older adults to manage heart disease, diabetes or obesity. About half of adults with heart disease (49%) or diabetes (47%) have arthritis, as do one-third (31%) of those who are obese. About half the adults with arthritis who also have heart disease, diabetes or obesity, have some limitation of their normal activities because of their arthritis. These patients might also have more challenges with their medications, especially if they take medicines for their heart disease, diabetes or other diseases. This boosts their chances of a bad reaction to the medicine.
Inflammatory arthritis (IA) actually drives multi-morbidity (heart, stroke, chronic lung disease, osteoporosis). A related concern is that older adults diagnosed with IA tend to be treated less aggressively than younger IA patients. For example, while methotrexate use among older rheumatoid arthritis patients is slightly higher compared to younger patients, the dosage is generally lower. Similarly, the percentage of older adults on multiple DMARDs or receiving biologic medications is lower than in younger patients, even though these drugs (biologics in particular) have been shown to have similar efficacy in older and younger individuals.
A major factor, for example, for the less widespread use of DMARDs among adults with elderly onset of rheumatoid arthritis (EORA) is the concern of physicians and patients that drug-related side effects may occur. Infections that may develop due to the use of DMARDs are more complicated and serious in older patients compared with younger patients and this is a concern of many physicians. However, many studies in recent years have shown that DMARD-related toxicity in older patients is low and comparable to younger patients. So, even in patients with EORA, DMARD treatment should be started quickly.
 Looking at gender
Looking at gender
Many types of arthritis are more common in women, including OA and rheumatoid arthritis (RA). However, gout is more common in men.
Why women?
The reasons for these differences between men and women are not completely understood. According to the “Life with arthritis in Canada” study, several factors, such as longer life expectancy, hormones and lifestyle differences, may explain the higher prevalence of arthritis among women.
Research indicates that hormonal differences may be one reason why women’s joints are susceptible to injury. Estrogen is a key hormone, which makes women, women. Among other functions, estrogen protects cartilage in joints and increases production of its two important building blocks: collagen and proteoglycans. After menopause, there is a steep drop-off in a woman’s protective estrogen level, leaving joints deprived of these strengthening molecules. Day-to-day stress on the knee, along with repeated bumps and bruises can now make joints prone to long-term damage and osteoarthritis.
Growth factors promote tissue regrowth and are important in repairing the damage that occurs from daily activities. Scientific research indicates that levels of growth factors are significantly decreased in women with severe osteoarthritis. Women thus have a lower ability to repair soft tissue damage and end up with more severe cartilage damage.
A Mayo Clinic study found that a contributing environmental factor for rheumatoid arthritis (RA) could include the changing composition of oral contraceptives. The pill has been shown to protect women against RA. However, because the oral contraceptives of today contain far less estrogen than they used to, they may be less protective.
Vitamin D deficiency is more severe in women and has been linked to higher rates of women having RA. A 2016 meta-analysis of 15 studies involving more than 2,000 people found that vitamin D deficiency was more prevalent and blood levels significantly lower among RA patients than those without RA. Patients with the lowest levels also had the most severe disease.
According to data presented at the American College of Rheumatology Annual Scientific Meeting in November 2021, the use of vitamin D3 or omega-3 fatty acid supplements over a 5-year period may reduce the incidence* of autoimmune disease (including RA) in older adults by 25% to 30%, according to data presented at ACR Convergence 2021.
*(Incidence is a measure of disease that allows us to determine a person’s probability of being diagnosed with a disease during a given period of time. Therefore, incidence is the number of newly diagnosed cases of a disease.)
“In past studies, inflammatory bowel disease, multiple sclerosis and type 2 diabetes have been shown to be more prevalent at northern latitudes, where circulating vitamin D levels are lower,” Karen Costenbader, MD, MPH, director of the Lupus Program at Brigham and Women’s Hospital, told attendees at the ACR meeting. “Both vitamin D and high residential UV exposure were associated with a decreased risk for rheumatoid arthritis among women in the Nurses’ Health Study in our past work.”
Dr. Costenbader’s team of researchers found a more pronounced effect after 2 to 3 years of use with vitamin D makes sense biologically and supports long-term use: “There is an ongoing extension study confirming incident cases in further follow-up. The clinical importance of these results is very high given that these are well-tolerated, non-toxic supplements, and that there are no other known effective therapies to reduce incidence for autoimmune diseases,” explained Dr. Costenbader.
 Genetics
Genetics
Genetics is another risk factor for arthritis that you cannot control. Individuals with specific genes are more likely to develop certain types of arthritis, such as RA, lupus, and spondyloarthritis. These genes are called HLA (human leukocyte antigen) class II genotypes. Experts do not fully understand why people with certain genes are at higher risk for developing arthritis or why it can make their arthritis worse.
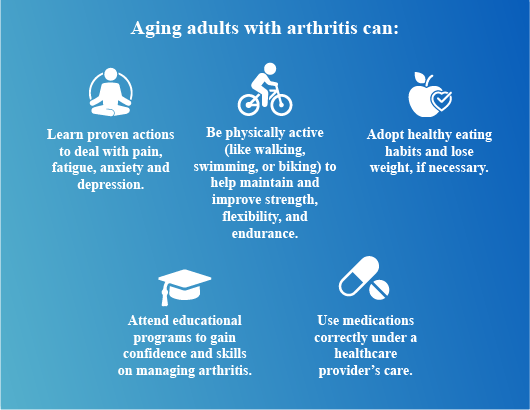
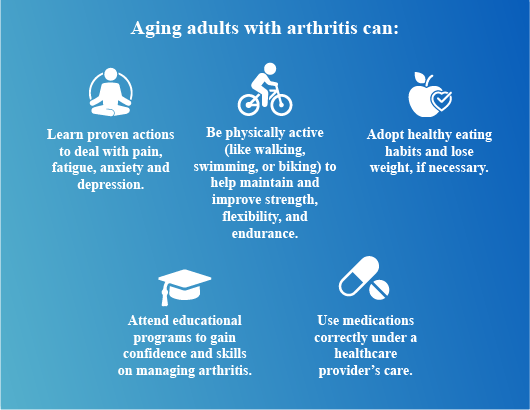
Yes, you can: Taking control of your arthritis
Here are several important steps in self-care to help older adults control their arthritis:
 Diet and nutrition
Diet and nutrition
Eating whole foods can help manage symptoms of arthritis. The Canada Food Guide recommends:
Unfortunately, there is no “magic arthritis diet” that can cure a person’s arthritis or eliminate arthritis symptoms. Unproven diets, or “miracle cures”, are commonly found on the internet, and rumors abound about certain foods to eliminate or eat in excess. It is important to remember that few of these theories have ever been scientifically examined, and none have been scientifically proven effective.
Though no dietary miracles have yet been discovered in the fight against arthritis, scientists have made several recent research advancements on the role of diet and nutrition in arthritis treatment. Today, we understand much more about the connections between arthritis, diet, healthy bodyweight, immune function, and inflammation. We are learning more and more about the positive steps each of us can take to fight arthritis and encourage overall health.
To help you understand what the research is telling us about arthritis and diet and nutrition, ACE has created a summary what is proven effective, and what is not.
 Exercise as medicine
Exercise as medicine
Arthritis aches and pains are not a normal part of aging. Physical activity can reduce pain and improve function by helping to lubricate joints and strengthen supporting structures such as muscles, tendons, and ligaments to help better distribute load. Regular movement has also been shown to boost mood and regulate inflammatory responses. Best part of all, physical activity does not need to be structured. Consider morning stretches in bed, a walking coffee date with a friend, dancing while you cook, cleaning or gardening.
Whenever starting something new, remember to give your body time to adjust. Consult your physician before starting an exercise plan. And remember: “slow and steady” and “consistency is key”.
To learn more about the benefits of exercise and what types of exercise to consider, please listen to a JointHealth™ podcast with Dr. Linda Li, Professor at the School of Rehabilitation Sciences, University of British Columbia. In the podcast, Dr. Li looks at the benefits of exercise for osteoarthritis, rheumatoid arthritis, ankylosing spondylitis, and psoriatic arthritis, including:
No smoking, please
Smoking is linked to the development of rheumatoid arthritis (RA), particularly for people who have smoked 20 years or longer. Smokers also have an increased risk of more-severe RA. In addition, they may be less likely to experience remission.
Smoking decreases the effectiveness of some medications used to treat RA and can be a barrier to engaging in activities that may relieve symptoms of rheumatoid arthritis, such as exercise, which is an important part of managing RA.
The exact reason why smoking is linked to RA isn’t well understood, but researchers suspect smoking somehow ignites faulty immune system functioning in people genetically predisposed to getting rheumatoid arthritis.
If you are considering quitting smoking or another tobacco product, click here to access free and convenient support from your province or territory in Canada.
 Getting social, avoiding isolation
Getting social, avoiding isolation
Research has shown the importance for older adults living with arthritis to build a social network and allow others to support you. Support from groups or from peer-to-peer contact can improve mood, provide better coping skills, decrease pain and provide relief from negative emotions, such as fear, resentment and hopelessness, according to Dr. Vicki Helgeson, of Carnegie-Mellon University, who has studied the impact of support groups for more than a decade.
For example, an educational group moderated by professionals sets a formal pace, while peer or self-help groups are open-ended and run by a participant. “I found that peer discussion groups work best for people who lack support at home,” says Helgeson, noting that for people who do have significant support systems in place, an educational support group might be of greater use.
The internet can be a powerful and empowering research and communication tool for the older adult with arthritis. Arthritis Consumer Experts provides links to websites that are useful in arthritis education, self-management and connecting with patients like you. Click here for a list of resources for both provincial, national, and international support.
 Sleepless in arthritis
Sleepless in arthritis
As many older arthritis patients know, sleep and immunity are partners in sickness and health. According to Dr. Michael Irwin, director of the Mindful Awareness Research Center at the University of California, Los Angeles: “Both sleep disturbance — that is, the quality of one’s sleep — and duration, are both associated with mortality risk and increases in the incidence and severity of immune-mediated inflammatory diseases.”
According to Irwin, inadequate sleep may have impacts on TNF, interleukin (IL)-6 and C-reactive protein levels. It is because of these impacts that sleep disturbance is not only a consequence of inflammation, but a driver of inflammation.
Irwin concluded by stressing that sleep disturbance can have as significant impacts on inflammation and antiviral immunity as poor diet, sedentary activity and obesity. “Treatments that target sleep behaviors reduce inflammation and improve antiviral immunity could possibly mitigate risk of inflammatory disorders and infectious disease risk,” he said.
Tips for better sleep
Getting to sleep, and staying that way, can be very difficult, especially for older people who live with arthritis and experience chronic pain. If your goal is to sleep better, here’s what you can do: Get involved in sleep research
Get involved in sleep research
Researchers at the University of British Columbia, McGill University, and Arthritis Research Canada are conducting research to learn more about sleep in persons with arthritis. The survey results will help tailor an online cognitive-behavioral program to help individuals with arthritis improve their sleep.
If you are interested in participating, please click here to open a new page with the consent form and survey.
Listening to you
We hope you find this information of use. Please tell us what you think by writing to us or emailing us at feedback@jointhealth.org. Through your ongoing and active participation, ACE can make its work more relevant to all Canadians living with arthritis.
Update your email or postal address
Please let us know of any changes by contacting ACE at feedback@jointhealth.org. This will ensure that you continue to receive your free email or print copy of JointHealth™ insight.
Arthritis Consumer Experts (ACE)
Who We Are
Arthritis Consumer Experts (ACE) and its team members acknowledge that they gather and work on the traditional, ancestral and unceded territory of the Coast Salish peoples -ʷməθkʷəy̓əm (Musqueam), Sḵwx̱wú7mesh (Squamish), and Səl̓ílwətaʔ/Selilwitulh (Tsleil-Waututh) Nations.
Arthritis Consumer Experts (ACE) operates as a non-profit and provides free research based education and information to Canadians with arthritis. We help (em)power people living with all forms of arthritis to take control of their disease and to take action in healthcare and research decision making. ACE activities are guided by its members and led by people with arthritis, scientific and medical experts on the ACE Advisory Board. To learn more about ACE, visit www.jointhealth.org
Disclosures
Over the past 12 months, ACE received grants-in-aid from: Arthritis Research Canada, Amgen Canada, Canadian Biosimilars Forum, Canadian Institutes of Health Research, Canadian Rheumatology Association, Eli Lilly Canada, Fresenius Kabi Canada, Gilead Sciences Canada, Hoffman-La Roche Canada Ltd., Knowledge Translation Canada, Merck Canada, Novartis Canada, Pfizer Canada, Sandoz Canada, Sanofi Canada, St. Paul's Hospital (Vancouver), Teva Canada, UCB Canada, and the University of British Columbia.
ACE also received unsolicited donations from its community members (people with arthritis) across Canada.
ACE thanks funders for their support to help the nearly 6 million Canadians living with osteoarthritis, rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis and the many other forms of the disease.
Disclaimer
The material contained on this website is provided for general information only. This website should not be relied on to suggest a course of treatment for a particular individual or as a substitute for consultation with qualified health professionals who are familiar with your individual medical needs. Should you have any healthcare related questions, you should contact your physician. You should never disregard medical advice or delay in seeking it because of something you have read on this or any website.
This site may provide links to other Internet sites only for the convenience of World Wide Web users. ACE is not responsible for the availability or content of these external sites, nor does ACE endorse, warrant or guarantee the products, services or information described or offered at these other Internet sites.
Although the information presented on this website is believed to be accurate at the time it is posted, this website could include inaccuracies, typographical errors or out-of-date information. This website may be changed at any time without prior notice.


 In a 2021 national survey, Arthritis Consumer Experts (ACE) attempted to identify inequities and gaps in arthritis self-advocacy – who is experiencing them and what some of the challenges are in advocating for the best arthritis care possible. One of the key insights that many respondents shared was a desire to learn more about aging and arthritis.
In a 2021 national survey, Arthritis Consumer Experts (ACE) attempted to identify inequities and gaps in arthritis self-advocacy – who is experiencing them and what some of the challenges are in advocating for the best arthritis care possible. One of the key insights that many respondents shared was a desire to learn more about aging and arthritis.In this issue of JointHealth™ insight, we look at the complex relationship between aging and arthritis.
It’s one of the biggest misconceptions about arthritis. Most people believe that arthritis is an old person’s disease and that it is entirely a consequence of aging. If that were the case, arthritis would be inevitable — and it’s not.
There are more than 100 different types of arthritis, a disease that affects people of all ages, from babies to older adults; in fact, more than three in five people diagnosed with arthritis are under the age of 65.
One of the reasons people assume arthritis is an inevitable consequence of aging is that the risk of developing the most common type of arthritis, osteoarthritis, increases with age. The risk of developing osteoporosis, a condition often confused with osteoarthritis, also increases with age. While the risk of developing osteoarthritis increases with age, keep in mind that it is not the only contributing factor:
- Osteoarthritis onset usually occurs after the age of 40; known risk factors include trauma from knee or hip injury.
- Rheumatoid arthritis, an autoimmune inflammatory type of arthritis, can develop at any age.
- Ankylosing spondylitis is most common in people between ages 15 and 40.
- Systemic lupus erythematosus usually develops between infancy and old age, with a peak occurrence between 15 to 40 years of age.
- Fibromyalgia is typically diagnosed in middle age and prevalence increases with age.
- Juvenile idiopathic arthritis occurs in people up to 16 years of age.
 Age and other risk factors for arthritis
Age and other risk factors for arthritisLet’s now look at aging and other risk factors for arthritis and ways to prevent and live your best with arthritis.
Aging with arthritis
With aging of the population, the number of older adults evaluated in rheumatology clinics is expected to increase dramatically in Canada and the rest of the world. Age is a primary risk factor for most types of arthritis, and increases as you get older. For example, as the population ages, osteoarthritis (OA) becomes more common. Your weight is the biggest modifiable risk factor for developing OA as excess weight places additional stress on weight-bearing joints in your hip and knee.
Researchers have also identified numerous contributing factors for “elderly onset” of inflammatory arthritis, including smoking, periodontitis, and viral infections. There may also be an association with menopause and hormonal changes.
Older arthritis patients are at higher risk than younger patients for falls and decline in the ability to perform daily physical activities such as holding a cup, lifting a grocery bag, or walking to a car. This emphasizes the importance of early diagnosis and treatment for older arthritis patients to prevent these complications.
At the 2021 American College of Rheumatology annual scientific conference, researchers shared presentations at a Scientific Study session – “Multicomplexity in the Aging Patient with Rheumatoid Arthritis” - on how to improve the models of care for older patients. These researchers stressed how important it is for rheumatologists and arthritis health professionals to be aware of issues such as multimorbidity (patient with two or more chronic diseases) and polypharmacy (the use of multiple medicines that is common in older patient populations with multimorbidities) that pose unique challenges and barriers to outcomes for older patients.
For example, arthritis can make it harder for older adults to manage heart disease, diabetes or obesity. About half of adults with heart disease (49%) or diabetes (47%) have arthritis, as do one-third (31%) of those who are obese. About half the adults with arthritis who also have heart disease, diabetes or obesity, have some limitation of their normal activities because of their arthritis. These patients might also have more challenges with their medications, especially if they take medicines for their heart disease, diabetes or other diseases. This boosts their chances of a bad reaction to the medicine.
Inflammatory arthritis (IA) actually drives multi-morbidity (heart, stroke, chronic lung disease, osteoporosis). A related concern is that older adults diagnosed with IA tend to be treated less aggressively than younger IA patients. For example, while methotrexate use among older rheumatoid arthritis patients is slightly higher compared to younger patients, the dosage is generally lower. Similarly, the percentage of older adults on multiple DMARDs or receiving biologic medications is lower than in younger patients, even though these drugs (biologics in particular) have been shown to have similar efficacy in older and younger individuals.
A major factor, for example, for the less widespread use of DMARDs among adults with elderly onset of rheumatoid arthritis (EORA) is the concern of physicians and patients that drug-related side effects may occur. Infections that may develop due to the use of DMARDs are more complicated and serious in older patients compared with younger patients and this is a concern of many physicians. However, many studies in recent years have shown that DMARD-related toxicity in older patients is low and comparable to younger patients. So, even in patients with EORA, DMARD treatment should be started quickly.
 Looking at gender
Looking at genderMany types of arthritis are more common in women, including OA and rheumatoid arthritis (RA). However, gout is more common in men.
Why women?
The reasons for these differences between men and women are not completely understood. According to the “Life with arthritis in Canada” study, several factors, such as longer life expectancy, hormones and lifestyle differences, may explain the higher prevalence of arthritis among women.
Research indicates that hormonal differences may be one reason why women’s joints are susceptible to injury. Estrogen is a key hormone, which makes women, women. Among other functions, estrogen protects cartilage in joints and increases production of its two important building blocks: collagen and proteoglycans. After menopause, there is a steep drop-off in a woman’s protective estrogen level, leaving joints deprived of these strengthening molecules. Day-to-day stress on the knee, along with repeated bumps and bruises can now make joints prone to long-term damage and osteoarthritis.
Growth factors promote tissue regrowth and are important in repairing the damage that occurs from daily activities. Scientific research indicates that levels of growth factors are significantly decreased in women with severe osteoarthritis. Women thus have a lower ability to repair soft tissue damage and end up with more severe cartilage damage.
A Mayo Clinic study found that a contributing environmental factor for rheumatoid arthritis (RA) could include the changing composition of oral contraceptives. The pill has been shown to protect women against RA. However, because the oral contraceptives of today contain far less estrogen than they used to, they may be less protective.
Vitamin D deficiency is more severe in women and has been linked to higher rates of women having RA. A 2016 meta-analysis of 15 studies involving more than 2,000 people found that vitamin D deficiency was more prevalent and blood levels significantly lower among RA patients than those without RA. Patients with the lowest levels also had the most severe disease.
According to data presented at the American College of Rheumatology Annual Scientific Meeting in November 2021, the use of vitamin D3 or omega-3 fatty acid supplements over a 5-year period may reduce the incidence* of autoimmune disease (including RA) in older adults by 25% to 30%, according to data presented at ACR Convergence 2021.
*(Incidence is a measure of disease that allows us to determine a person’s probability of being diagnosed with a disease during a given period of time. Therefore, incidence is the number of newly diagnosed cases of a disease.)
“In past studies, inflammatory bowel disease, multiple sclerosis and type 2 diabetes have been shown to be more prevalent at northern latitudes, where circulating vitamin D levels are lower,” Karen Costenbader, MD, MPH, director of the Lupus Program at Brigham and Women’s Hospital, told attendees at the ACR meeting. “Both vitamin D and high residential UV exposure were associated with a decreased risk for rheumatoid arthritis among women in the Nurses’ Health Study in our past work.”
Dr. Costenbader’s team of researchers found a more pronounced effect after 2 to 3 years of use with vitamin D makes sense biologically and supports long-term use: “There is an ongoing extension study confirming incident cases in further follow-up. The clinical importance of these results is very high given that these are well-tolerated, non-toxic supplements, and that there are no other known effective therapies to reduce incidence for autoimmune diseases,” explained Dr. Costenbader.
 Genetics
GeneticsGenetics is another risk factor for arthritis that you cannot control. Individuals with specific genes are more likely to develop certain types of arthritis, such as RA, lupus, and spondyloarthritis. These genes are called HLA (human leukocyte antigen) class II genotypes. Experts do not fully understand why people with certain genes are at higher risk for developing arthritis or why it can make their arthritis worse.
Yes, you can: Taking control of your arthritis
Here are several important steps in self-care to help older adults control their arthritis:
 Diet and nutrition
Diet and nutritionEating whole foods can help manage symptoms of arthritis. The Canada Food Guide recommends:
- Seven to 10 servings of vegetables and fruits each day. Pick lots of bright orange and green options, such as broccoli, cantaloupe and carrots. They are high in antioxidants, which may reduce inflammation, decrease cartilage breakdown and slow the progress of osteoarthritis.
- Choose more whole grains such as brown rice, barley and oats. They have more antioxidants than refined grains, such as white bread and white rice.
- Choose more unsaturated fats like canola and olive oil, nuts like walnuts and almonds and fish like salmon. Enjoy saturated and trans-fat like butter, lard, cream, baked goods and fried foods in moderation.
Unfortunately, there is no “magic arthritis diet” that can cure a person’s arthritis or eliminate arthritis symptoms. Unproven diets, or “miracle cures”, are commonly found on the internet, and rumors abound about certain foods to eliminate or eat in excess. It is important to remember that few of these theories have ever been scientifically examined, and none have been scientifically proven effective.
Though no dietary miracles have yet been discovered in the fight against arthritis, scientists have made several recent research advancements on the role of diet and nutrition in arthritis treatment. Today, we understand much more about the connections between arthritis, diet, healthy bodyweight, immune function, and inflammation. We are learning more and more about the positive steps each of us can take to fight arthritis and encourage overall health.
To help you understand what the research is telling us about arthritis and diet and nutrition, ACE has created a summary what is proven effective, and what is not.
 Exercise as medicine
Exercise as medicineArthritis aches and pains are not a normal part of aging. Physical activity can reduce pain and improve function by helping to lubricate joints and strengthen supporting structures such as muscles, tendons, and ligaments to help better distribute load. Regular movement has also been shown to boost mood and regulate inflammatory responses. Best part of all, physical activity does not need to be structured. Consider morning stretches in bed, a walking coffee date with a friend, dancing while you cook, cleaning or gardening.
Whenever starting something new, remember to give your body time to adjust. Consult your physician before starting an exercise plan. And remember: “slow and steady” and “consistency is key”.
To learn more about the benefits of exercise and what types of exercise to consider, please listen to a JointHealth™ podcast with Dr. Linda Li, Professor at the School of Rehabilitation Sciences, University of British Columbia. In the podcast, Dr. Li looks at the benefits of exercise for osteoarthritis, rheumatoid arthritis, ankylosing spondylitis, and psoriatic arthritis, including:
- types of safe exercise for the person with arthritis
- protecting one’s joints during exercise
- preparing to exercise safely (joint protection, warm up/cool down, etc.)
- after exercise strategies to prevent joint pain and stiffness
No smoking, please
Smoking is linked to the development of rheumatoid arthritis (RA), particularly for people who have smoked 20 years or longer. Smokers also have an increased risk of more-severe RA. In addition, they may be less likely to experience remission.
Smoking decreases the effectiveness of some medications used to treat RA and can be a barrier to engaging in activities that may relieve symptoms of rheumatoid arthritis, such as exercise, which is an important part of managing RA.
The exact reason why smoking is linked to RA isn’t well understood, but researchers suspect smoking somehow ignites faulty immune system functioning in people genetically predisposed to getting rheumatoid arthritis.
If you are considering quitting smoking or another tobacco product, click here to access free and convenient support from your province or territory in Canada.
 Getting social, avoiding isolation
Getting social, avoiding isolationResearch has shown the importance for older adults living with arthritis to build a social network and allow others to support you. Support from groups or from peer-to-peer contact can improve mood, provide better coping skills, decrease pain and provide relief from negative emotions, such as fear, resentment and hopelessness, according to Dr. Vicki Helgeson, of Carnegie-Mellon University, who has studied the impact of support groups for more than a decade.
For example, an educational group moderated by professionals sets a formal pace, while peer or self-help groups are open-ended and run by a participant. “I found that peer discussion groups work best for people who lack support at home,” says Helgeson, noting that for people who do have significant support systems in place, an educational support group might be of greater use.
The internet can be a powerful and empowering research and communication tool for the older adult with arthritis. Arthritis Consumer Experts provides links to websites that are useful in arthritis education, self-management and connecting with patients like you. Click here for a list of resources for both provincial, national, and international support.
 Sleepless in arthritis
Sleepless in arthritisAs many older arthritis patients know, sleep and immunity are partners in sickness and health. According to Dr. Michael Irwin, director of the Mindful Awareness Research Center at the University of California, Los Angeles: “Both sleep disturbance — that is, the quality of one’s sleep — and duration, are both associated with mortality risk and increases in the incidence and severity of immune-mediated inflammatory diseases.”
According to Irwin, inadequate sleep may have impacts on TNF, interleukin (IL)-6 and C-reactive protein levels. It is because of these impacts that sleep disturbance is not only a consequence of inflammation, but a driver of inflammation.
Irwin concluded by stressing that sleep disturbance can have as significant impacts on inflammation and antiviral immunity as poor diet, sedentary activity and obesity. “Treatments that target sleep behaviors reduce inflammation and improve antiviral immunity could possibly mitigate risk of inflammatory disorders and infectious disease risk,” he said.
Tips for better sleep
Getting to sleep, and staying that way, can be very difficult, especially for older people who live with arthritis and experience chronic pain. If your goal is to sleep better, here’s what you can do:
- Keep a regular sleep-wake pattern. Try to go to bed at the same time each night and wake up around the same time each morning.
- Avoid alcohol and caffeine in the late afternoon and evening. Though alcohol can make you sleepy, it can disrupt sleep as well.
- If you need to nap during the day, keep it short; under an hour is best.
- Keep your bedroom only for sleeping – avoid activities like watching television, eating, and working on your computer in your bedroom.
- Exercise regularly but avoid doing so for at least three hours before bed, as exercise can be stimulating, as opposed to relaxing.
- Learn mindfulness and meditation techniques.
- Keep your bedroom cool and dark.
- Fresh air is important; if possible, sleep with a window slightly open.
- Take time to relax before bed – take a warm bath, listen to soothing music, drink chamomile tea, or read a relaxing book.
- Make sure your mattress and pillows are of a firmness which is comfortable to you. Experiment with pillow type and positioning to find a set-up which works for you. Look into the many different types of pillows on the market, including wedge-shaped pillows and body pillows.
- Control your pain at nighttime; talk to your doctor about adjusting your pain medication schedule so that your pain is relieved at night.
 Get involved in sleep research
Get involved in sleep researchResearchers at the University of British Columbia, McGill University, and Arthritis Research Canada are conducting research to learn more about sleep in persons with arthritis. The survey results will help tailor an online cognitive-behavioral program to help individuals with arthritis improve their sleep.
If you are interested in participating, please click here to open a new page with the consent form and survey.
Listening to you
We hope you find this information of use. Please tell us what you think by writing to us or emailing us at feedback@jointhealth.org. Through your ongoing and active participation, ACE can make its work more relevant to all Canadians living with arthritis.
Update your email or postal address
Please let us know of any changes by contacting ACE at feedback@jointhealth.org. This will ensure that you continue to receive your free email or print copy of JointHealth™ insight.
Arthritis Consumer Experts (ACE)
Who We Are
Arthritis Consumer Experts (ACE) and its team members acknowledge that they gather and work on the traditional, ancestral and unceded territory of the Coast Salish peoples -ʷməθkʷəy̓əm (Musqueam), Sḵwx̱wú7mesh (Squamish), and Səl̓ílwətaʔ/Selilwitulh (Tsleil-Waututh) Nations.
Arthritis Consumer Experts (ACE) operates as a non-profit and provides free research based education and information to Canadians with arthritis. We help (em)power people living with all forms of arthritis to take control of their disease and to take action in healthcare and research decision making. ACE activities are guided by its members and led by people with arthritis, scientific and medical experts on the ACE Advisory Board. To learn more about ACE, visit www.jointhealth.org
Disclosures
Over the past 12 months, ACE received grants-in-aid from: Arthritis Research Canada, Amgen Canada, Canadian Biosimilars Forum, Canadian Institutes of Health Research, Canadian Rheumatology Association, Eli Lilly Canada, Fresenius Kabi Canada, Gilead Sciences Canada, Hoffman-La Roche Canada Ltd., Knowledge Translation Canada, Merck Canada, Novartis Canada, Pfizer Canada, Sandoz Canada, Sanofi Canada, St. Paul's Hospital (Vancouver), Teva Canada, UCB Canada, and the University of British Columbia.
ACE also received unsolicited donations from its community members (people with arthritis) across Canada.
ACE thanks funders for their support to help the nearly 6 million Canadians living with osteoarthritis, rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis and the many other forms of the disease.
Disclaimer
The material contained on this website is provided for general information only. This website should not be relied on to suggest a course of treatment for a particular individual or as a substitute for consultation with qualified health professionals who are familiar with your individual medical needs. Should you have any healthcare related questions, you should contact your physician. You should never disregard medical advice or delay in seeking it because of something you have read on this or any website.
This site may provide links to other Internet sites only for the convenience of World Wide Web users. ACE is not responsible for the availability or content of these external sites, nor does ACE endorse, warrant or guarantee the products, services or information described or offered at these other Internet sites.
Although the information presented on this website is believed to be accurate at the time it is posted, this website could include inaccuracies, typographical errors or out-of-date information. This website may be changed at any time without prior notice.
