In this issue
- Background
- Advocating to your healthcare provider
- Explaining arthritis to the people in your world
- Survey respondent characteristics
- Where respondents live
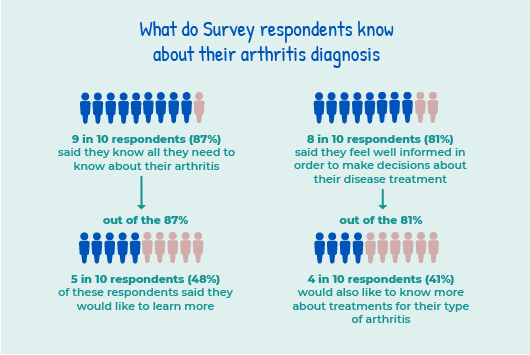
- What do Survey respondents know about their arthritis diagnosis
- What is statistical significance?
- The link between emotional support and mental health
- Work and arthritis
- The challenges of living with arthritis
- Getting information on arthritis
- Respondents and their health care teams
- Reaching out to the community
- Discussion
- Resources for arthritis self-advocacy
JointHealth™ insight Published September 2021
 One of the most important voices in discussions about arthritis care belongs to those most affected by health policy – the person living with arthritis. No one knows arthritis better than those who live with it every day. When you share your story and experiences with family and friends, your healthcare team, work colleagues, community leaders, and elected officials, you help them understand how their actions affect you.
One of the most important voices in discussions about arthritis care belongs to those most affected by health policy – the person living with arthritis. No one knows arthritis better than those who live with it every day. When you share your story and experiences with family and friends, your healthcare team, work colleagues, community leaders, and elected officials, you help them understand how their actions affect you.
 Arthritis Consumer Experts (ACE) conducted a national Survey from June 23 to July 24, 2021 to identify inequities and gaps in arthritis self-advocacy – who is experiencing them and what some of the challenges are in advocating for the best arthritis care possible.
Arthritis Consumer Experts (ACE) conducted a national Survey from June 23 to July 24, 2021 to identify inequities and gaps in arthritis self-advocacy – who is experiencing them and what some of the challenges are in advocating for the best arthritis care possible.
Background
When a person receives a diagnosis for a type of arthritis, a new journey starts and their role as self-advocate immediately begins.
This new role begins with being an informed self-advocate for the effects your disease has on your quality of life and the health care you receive from your healthcare team and the healthcare system. Self-advocacy can help give patients some stability, a feeling of regaining control and the strategies and tools to live your best life. Self-advocacy is a way of reaching out to others and explaining your arthritis experience to your family, friends, co-workers, employers, and even strangers and learning how to ask for support and help. Ultimately, self-advocacy requires participation in the decision-making process, particularly as it relates to the healthcare you receive.

Listening to you
We hope you find this information of use. Please tell us what you think by writing to us or emailing us at feedback@jointhealth.org. Through your ongoing and active participation, ACE can make its work more relevant to all Canadians living with arthritis.
Update your email or postal address
Please let us know of any changes by contacting ACE at feedback@jointhealth.org. This will ensure that you continue to receive your free email or print copy of JointHealth™ insight.
Arthritis Consumer Experts (ACE)
Who We Are
Arthritis Consumer Experts (ACE) and its team members acknowledge that they gather and work on the traditional, ancestral and unceded territory of the Coast Salish peoples -ʷməθkʷəy̓əm (Musqueam), Sḵwx̱wú7mesh (Squamish), and Səl̓ílwətaʔ/Selilwitulh (Tsleil-Waututh) Nations.
Arthritis Consumer Experts (ACE) operates as a non-profit and provides free research based education and information to Canadians with arthritis. We help (em)power people living with all forms of arthritis to take control of their disease and to take action in healthcare and research decision making. ACE activities are guided by its members and led by people with arthritis, scientific and medical experts on the ACE Advisory Board. To learn more about ACE, visit www.jointhealth.org
Disclosures
Over the past 12 months, ACE received grants-in-aid from: Arthritis Research Canada, Amgen Canada, Canadian Biosimilars Forum, Canadian Institutes of Health Research, Canadian Rheumatology Association, Eli Lilly Canada, Fresenius Kabi Canada, Gilead Sciences Canada, Hoffman-La Roche Canada Ltd., Knowledge Translation Canada, Merck Canada, Novartis Canada, Pfizer Canada, Sandoz Canada, Sanofi Canada, St. Paul's Hospital (Vancouver), Teva Canada, UCB Canada, and the University of British Columbia.
ACE also received unsolicited donations from its community members (people with arthritis) across Canada.
ACE thanks funders for their support to help the nearly 6 million Canadians living with osteoarthritis, rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis and the many other forms of the disease.
Disclaimer
The material contained on this website is provided for general information only. This website should not be relied on to suggest a course of treatment for a particular individual or as a substitute for consultation with qualified health professionals who are familiar with your individual medical needs. Should you have any healthcare related questions, you should contact your physician. You should never disregard medical advice or delay in seeking it because of something you have read on this or any website.
This site may provide links to other Internet sites only for the convenience of World Wide Web users. ACE is not responsible for the availability or content of these external sites, nor does ACE endorse, warrant or guarantee the products, services or information described or offered at these other Internet sites.
Although the information presented on this website is believed to be accurate at the time it is posted, this website could include inaccuracies, typographical errors or out-of-date information. This website may be changed at any time without prior notice.

Background
When a person receives a diagnosis for a type of arthritis, a new journey starts and their role as self-advocate immediately begins.
This new role begins with being an informed self-advocate for the effects your disease has on your quality of life and the health care you receive from your healthcare team and the healthcare system. Self-advocacy can help give patients some stability, a feeling of regaining control and the strategies and tools to live your best life. Self-advocacy is a way of reaching out to others and explaining your arthritis experience to your family, friends, co-workers, employers, and even strangers and learning how to ask for support and help. Ultimately, self-advocacy requires participation in the decision-making process, particularly as it relates to the healthcare you receive.

Advocating to your healthcare provider
Health research shows that people with arthritis and their healthcare providers (HCP) may each be speaking a “foreign language” to communicate what is important to each other.
For example, many ACE members living with an inflammatory arthritis have described how they define treatment success as no longer being in pain and having little to no inflammation, followed by improvement in their overall quality of life; while many healthcare providers state their goals for their patients are achieving disease remission and/or low disease activity.
While both patients and HCPs want to communicate clearly, a communication gap exists, and that gap results in some patients not getting the treatment results they and their healthcare team expect or desire. One Survey respondent commented: ”Sometimes, doctors have differing opinions on how to best deal with my arthritis. I will follow the rheumatologists’ advice and direct the disagreeing doctor to the specialist to discuss how best to handle my medications. Most disagreements have to do with the type and amount I need.” Explaining arthritis to the people in your world
Explaining arthritis to the people in your world
Arthritis is misunderstood – or not well understood – by the public. Most think “arthritis” is one disease when in fact there are over 100 different types. A self-advocacy challenge for a person living with arthritis is how to communicate your experience with family and friends, your co-workers and employer, as well as strangers you encounter and interact with daily.
To better understand patients’ understanding of their disease, where they go to learn about treatment and care, and how they go about self-advocating for what they need, ACE launched its third National Survey of 2021. Based on the insights from the Survey, ACE intends to develop education tools to help people living with arthritis communicate their lived experience at home and at work.
Methodology
An online survey of people who self-reported having a physician-diagnosed form of arthritis was conducted (June 23 to July 24, 2021) in English and French. The survey included 39 questions on respondents’ experiences with arthritis self-advocacy at work, in their social life, during medical appointments, and with mass media, Throughout the survey, respondents were able to provide additional comments about what would help improve their experience with arthritis self- advocacy. The data were aggregated, and global and subset analysis was performed by a data specialist.
Survey respondents' characteristics
Arthritis Consumer Experts received 322 responses, including 235 in English and 87 in French (85 were Quebec residents).
Respondents were people who self-reported living with various forms of arthritis, including:
Eight in 10 (82%) respondents identified as women and 2 in 10 (18%) identified as men.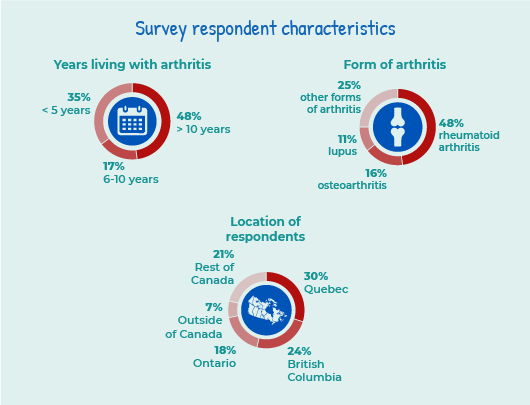
Where respondents live
The majority of Survey respondents reported living in Quebec (3 in 10 or 30%), followed by British Columbia (2 in 10 or 24%), and Ontario (2 in 10 or 18%). Seven per cent of respondents identified as living outside of Canada; including in the United States, Indonesia, the Philippines, Australia, and the United Kingdom. There were respondents from all Canadian provinces and territories except for Nunavut.
Respondents lived in both rural or small to medium sized, and urban communities:
Forty-four per cent of respondents travel 1-10km to see their rheumatologist, followed by:
To identify gaps in arthritis self-advocacy, we asked Survey respondents about their understanding of their type of arthritis and making treatment decisions. Nine in 10 or 87% respondents said they know all they need to about their arthritis – half or 48% of these respondents said they would also like to learn more. A similar number of people – 8 in 10 or 81% said they feel well informed in order to make decisions about their disease treatment. Out of the 81%; however, 4 in 10 or 41% would also like to know more about treatments for their type of arthritis.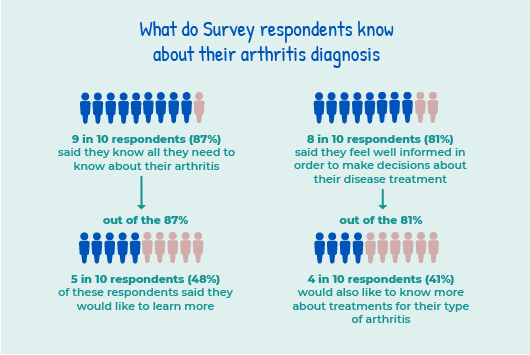
Survey respondent’s comfort level in asking their family members or friends for physical help with their type of arthritis
What respondents told us
When asked what specific types of information would help them know more about their arthritis diagnosis, here are a few answers in respondents’ own words:
“I would like to know the prognosis for each area of my body suffering the effects of arthritis so that I can recognize when interventions of differing types would be beneficial, e.g. arthritis in my thumb joint is increasingly impacting my ability to play the violin: so, when do I need to stop?”
“Learning about coexisting conditions and who to see to treat those symptoms. What is available for disease treatment and also pain relievers. Discussion on quality of life and needing to go on disability.”
“Literally as much as I can possibly learn. Possible causes, assistance, more about current and upcoming research, most importantly I have lots to learn about the supports I am eligible to receive in Canada and should seek out.”
In ACE’s Survey, we asked respondents who they ask or talk to for emotional support. Respondents were asked to select 3 answers from the list below, which is presented in rank order:
Seven in 10 respondents living in urban centres get emotional support from a friend. In comparison, 7 in 10 respondents living in rural and small to medium sized communities get emotional support from their spouse.
Findings were significantly different for respondents who identified as black, Indigenous, or a person of colour (BIPOC).
BIPOC respondents were:

The link between emotional support and mental health
Receiving physical or emotional support is particularly important for people with inflammatory arthritis (IA) who are more likely to experience mental health conditions such as depression, anxiety and “brain fog” than the general population. In fact, those living with rheumatoid arthritis are 17-20% more likely to develop depression.1
A key cause of mental health issues for people diagnosed with arthritis is the pain and disability associated with it. For example, new limitations caused by IA can bring significant changes to one’s life, work, relationships, leading to anxiety and depression. Researchers at the University of Glasgow found that chronic inflammation from IA, which affects joints and organs, such as the eyes, skin, and the brain, may also be related to mental health disorders like depression. “Brain fog” is another symptom of IA – it can create episode of confusion, disorientation and frustration.2
Conversations with friends and co-workers
In terms of sharing information about their disease, a majority of all respondents told their friends or co-workers about their arthritis diagnosis within a few weeks or months after receiving it.
ACE’s Survey also identified statistically significant differences among certain segments of respondents:
The Survey asked respondents if they know how to deal with physical limitations caused by their arthritis and that affect their ability to do their job – the majority of respondents answered yes (7 in 10 or 68%), followed by not sure (2 in 10 or 23%) and no (1 in 10 or 8%).
Respondents who identified as BIPOC were more likely to talk about their arthritis diagnosis with their employer than their non-BIPOC counterparts (3 in 4 or 76% compared to 5 in 10 or 55%).
ACE’s Survey also revealed statistical significance related to asking for and receiving job accommodations from an employer:
What respondents told us
ACE probed deeper on the topic of respondents’ experiences and asked them for their perspective on what made them comfortable (or uncomfortable) about sharing their arthritis diagnosis with their employer in their own words:
“Not until I needed surgery. I did not want to be discriminated against in the work place or considered “unable” to do anything or pull my weight. There is nothing worse than other people using your health condition as an excuse for not completing a task which you are collaborating with them on. If the job didn’t get done, it would not be because I have arthritis!”
“Prior bad experiences with employers when they found out. With new job, chose to tell immediate teammates first day, manager at first call after accepting the position. One challenge is having to have the conversation repeatedly as managers and teammates transition.”
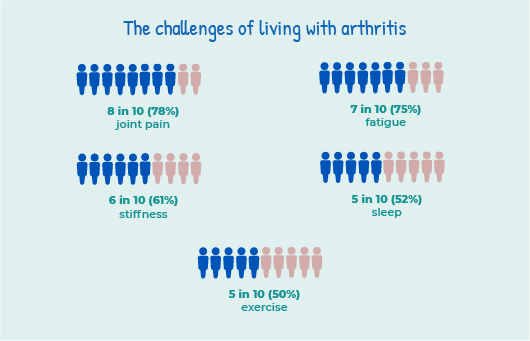
The challenges of living with arthritis
Respondents were asked to identify the most challenging things for them to deal with while living with their type of arthritis. They were able to select all that apply from a list – the top 5 answer choices were: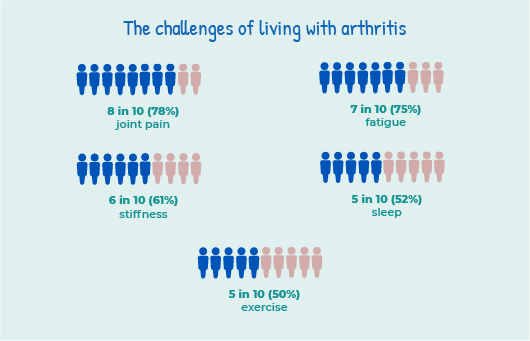
Getting information on arthritis
The Survey also asked respondents where they usually go to find information about their type of arthritis. The top 5 sources were:
ACE’s Survey also asked respondents what arthritis topics they most need information on. Respondents were asked to select 3 choices from the list below presented in rank order:

Respondents and their health care teams
Almost all (99%) of the respondents bring a list of questions or concerns they plan to discuss during their medical appointments. Similarly, 98% were confident about asking questions about their type of arthritis during a medical appointment and 99% were comfortable sharing their health concerns with the health care workers who provide care for their type of arthritis.
Eighty-five per cent of respondents found it “not that difficult” or “not difficult at all” to take action on the information and instructions given to them by their health professional caring for their type of arthritis versus 15% respondents who found it difficult.
What respondents told us
The Survey asked respondents what would help them feel more comfortable asking questions of their health care team members. Here’s what they told us in their own words:
“Written information. Written directions. Guidance on where to go for more information or help. Knowing that I can give them feed back on care directions & get responses. Knowing that there will be follow-up.”
“Generally, it depends on the attitude of the medical professional. If I feel rushed or that they are in a hurry to get to another appointment I won’t ask. Often I don’t have questions until I leave the office and have reflected on the information told to me, so maybe a way to email or contact someone about additional questions afterwards.”

Reaching out to the community
In its Survey, ACE wanted to find out the level of experience respondents had reaching out to members of their arthritis community to get information or share their story.
A surprising 67% of respondents have never asked a patient advocacy organization for help to get the things they need to live with their type of arthritis.
When it comes to sharing their experiences living with their type of arthritis through social media, key findings include:
Two in ten or 19% of respondents have shared their arthritis experiences with mainstream media (community papers, major newspaper, or TV).
What respondents told us
The Survey asked respondents what would make them feel more comfortable sharing their experiences with their type of arthritis through social media? Here’s what they said in their own words:
“Support from the community. Understanding. Compassion.”
“I’ve shared, however only through support groups of those with similar/same diagnosis as they are the most inclusive and supportive communities that I am part of.”
“I wasn’t comfortable at all actually. But I did share about a very specific experience I had on social media to get some traction with our local government about an arthritis program that was closing due to budget cuts.”
Discussion
Self-advocacy is the action of representing their experience, view or interests. For a person living with arthritis, self- advocacy and being an advocate first means being a part of your health care team. It means knowing yourself and speaking up for yourself to make sure that your arthritis care needs are met. A large majority of ACE’s Survey respondents report that they are actively working alongside their healthcare team to choose the best care and treatment for their type of arthritis. These findings suggest respondents know their bodies and understand what’s important to them, what they value and what their priorities are when they consider care and treatment options.
While the term self-advocacy implies advocating for yourself, by yourself, it doesn’t actually mean that you have to do it by yourself. ACE’s Survey respondents reported that many of them bring a friend or family member with them to their meetings with their healthcare team – not just to help take notes but to provide emotional support.
A support system is vital in practicing self-advocacy if you struggle with finding your voice and speaking up for yourself. A more outspoken family member or friend can give you a voice. The top three sources for emotional support cited by Survey respondents were close friend, spouse/partner and immediate family member. The ACE Survey findings also revealed a strong preference with a majority of respondents in terms of who they trust and turn to for information about their arthritis: respondents trusted the advice of their rheumatologist (76%), followed by family physician (8%) and other arthritis specialist and patient organizations (both at 7%).
Advocating at work
Arthritis is the leading cause of work disability in Canada. Arthritis typically occurs during prime working years, between ages 35-50.
ACE’s Survey found that respondents face particular challenges at work. Sixty-six per cent of non-BIPOC respondents said they have not asked for job accommodations. BIPOC respondents were 2 times more likely to experience challenges in advancing their career (33% compared to 17% of non-BIPOC).
Towards a better understanding of how you can advocate at work
Dr. Diane Lacaille of Arthritis Research Canada has conducted studies to determine what workplace factors are closely linked to the risk of a work disability lasting six months or longer.3
Dr. Lacaille found that high physical demand, low job independence (i.e. minimal control over the pace of work and how duties are performed) and poor support from co-workers aggravated arthritis symptoms and accounted for longer absences from work. If no obvious changes need to be made to your work space, your schedule, or your job position, you may decide not to tell people you have a serious type of inflammatory arthritis (IA), like rheumatoid arthritis, at all; there is no legal requirement for you to disclose your IA to your employer or fellow employees. Or perhaps you will begin with telling one or two trusted colleagues, as a way of testing the water and getting practice. It’s up to you. But do bear in mind that people who don’t know you have arthritis won’t know you may need support from time to time. And if at times you need to take frequent breaks or delegate certain tasks, resentment may build if people don’t know the reason and support you.
Flexible work schedules are particularly important for people with IA:
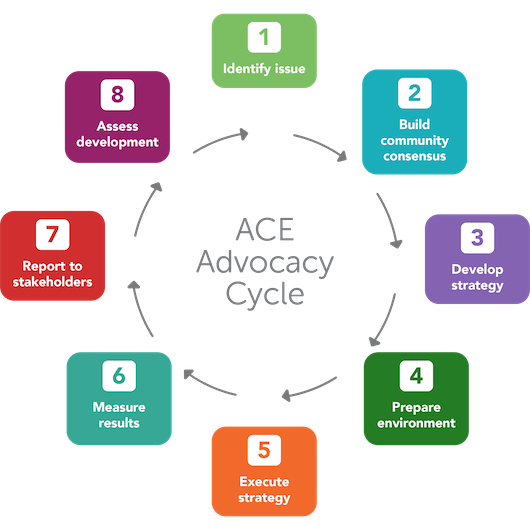
Resources for arthritis self-advocacy
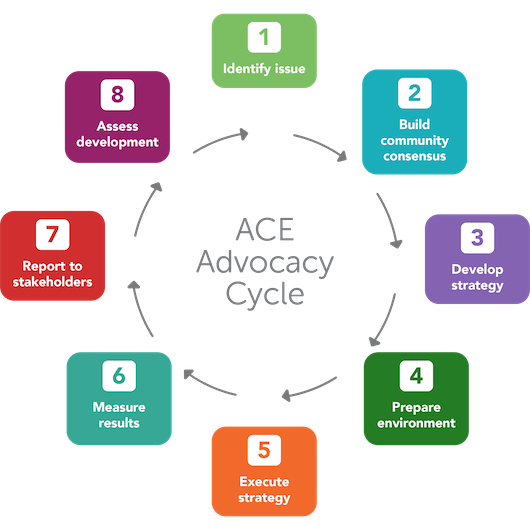
ACE’s advocacy cycle includes listening carefully to the issues, concerns, and experiences our members share with us. For example, the issue of how the voices of racial minorities are often underrepresented or excluded in health research. We then take that valuable information and create the messages and policy recommendations, find allies and supporters among patients and healthcare providers and deliver our arthritis story or “ask” to elected officials or the media. Here’s what ACE’s advocacy cycle looks like:
To help you on your journey with arthritis self-advocacy, the following ACE resources may be helpful:
References
Health research shows that people with arthritis and their healthcare providers (HCP) may each be speaking a “foreign language” to communicate what is important to each other.
For example, many ACE members living with an inflammatory arthritis have described how they define treatment success as no longer being in pain and having little to no inflammation, followed by improvement in their overall quality of life; while many healthcare providers state their goals for their patients are achieving disease remission and/or low disease activity.
While both patients and HCPs want to communicate clearly, a communication gap exists, and that gap results in some patients not getting the treatment results they and their healthcare team expect or desire. One Survey respondent commented: ”Sometimes, doctors have differing opinions on how to best deal with my arthritis. I will follow the rheumatologists’ advice and direct the disagreeing doctor to the specialist to discuss how best to handle my medications. Most disagreements have to do with the type and amount I need.”
 Explaining arthritis to the people in your world
Explaining arthritis to the people in your world Arthritis is misunderstood – or not well understood – by the public. Most think “arthritis” is one disease when in fact there are over 100 different types. A self-advocacy challenge for a person living with arthritis is how to communicate your experience with family and friends, your co-workers and employer, as well as strangers you encounter and interact with daily.
To better understand patients’ understanding of their disease, where they go to learn about treatment and care, and how they go about self-advocating for what they need, ACE launched its third National Survey of 2021. Based on the insights from the Survey, ACE intends to develop education tools to help people living with arthritis communicate their lived experience at home and at work.
| ACE’s National Survey on Arthritis Self-Advocacy |
An online survey of people who self-reported having a physician-diagnosed form of arthritis was conducted (June 23 to July 24, 2021) in English and French. The survey included 39 questions on respondents’ experiences with arthritis self-advocacy at work, in their social life, during medical appointments, and with mass media, Throughout the survey, respondents were able to provide additional comments about what would help improve their experience with arthritis self- advocacy. The data were aggregated, and global and subset analysis was performed by a data specialist.
| ACE extends its sincere thanks to the people who took time to participate in this important community-led research and to our community partners who helped promote the Survey. |
Arthritis Consumer Experts received 322 responses, including 235 in English and 87 in French (85 were Quebec residents).
Respondents were people who self-reported living with various forms of arthritis, including:
- rheumatoid arthritis (48%)
- osteoarthritis (16%)
- lupus (11%)
- psoriatic arthritis (7%)
- ankylosing spondylitis (3%)
- juvenile idiopathic arthritis (3%)
- other (3%)
- non-radiographic axial spondyloarthritis (2%)
- scleroderma (2%)
- do not know what type of arthritis they have (2%)
Eight in 10 (82%) respondents identified as women and 2 in 10 (18%) identified as men.
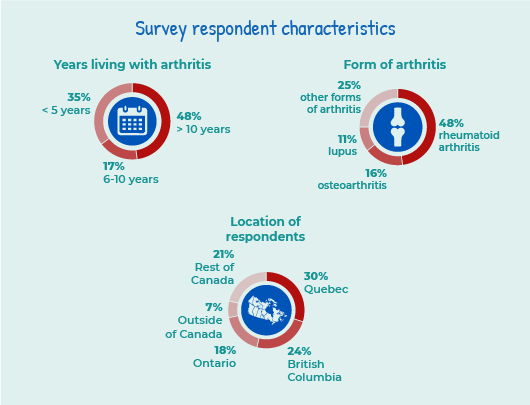
Where respondents live
The majority of Survey respondents reported living in Quebec (3 in 10 or 30%), followed by British Columbia (2 in 10 or 24%), and Ontario (2 in 10 or 18%). Seven per cent of respondents identified as living outside of Canada; including in the United States, Indonesia, the Philippines, Australia, and the United Kingdom. There were respondents from all Canadian provinces and territories except for Nunavut.
Respondents lived in both rural or small to medium sized, and urban communities:
- 65% of respondents live in large urban centres with population of 100,000 or more
- 35% of respondents live in either rural (population of 15,000 or less) or small to medium sized population centres (population of 16,000 to 99,999)
Forty-four per cent of respondents travel 1-10km to see their rheumatologist, followed by:
11-25km (25%)What do Survey respondents know about their arthritis diagnosis
26-50km (13%)
51-100km (7%)
101-250km (5%)
251-500km (4%)
500km or more (1%)
To identify gaps in arthritis self-advocacy, we asked Survey respondents about their understanding of their type of arthritis and making treatment decisions. Nine in 10 or 87% respondents said they know all they need to about their arthritis – half or 48% of these respondents said they would also like to learn more. A similar number of people – 8 in 10 or 81% said they feel well informed in order to make decisions about their disease treatment. Out of the 81%; however, 4 in 10 or 41% would also like to know more about treatments for their type of arthritis.
Survey respondent’s comfort level in asking their family members or friends for physical help with their type of arthritis
- Somewhat comfortable: 96 (35%)
- Very comfortable: 89 (32%)
- I’m not comfortable but I ask anyway: 55 (20%)
- I’m not comfortable asking for help so I don’t ask: 20 (7%)
- I’m not comfortable but would like to learn how to ask: 17 (6%)
What respondents told us
When asked what specific types of information would help them know more about their arthritis diagnosis, here are a few answers in respondents’ own words:
“I would like to know the prognosis for each area of my body suffering the effects of arthritis so that I can recognize when interventions of differing types would be beneficial, e.g. arthritis in my thumb joint is increasingly impacting my ability to play the violin: so, when do I need to stop?”
“Learning about coexisting conditions and who to see to treat those symptoms. What is available for disease treatment and also pain relievers. Discussion on quality of life and needing to go on disability.”
“Literally as much as I can possibly learn. Possible causes, assistance, more about current and upcoming research, most importantly I have lots to learn about the supports I am eligible to receive in Canada and should seek out.”
In ACE’s Survey, we asked respondents who they ask or talk to for emotional support. Respondents were asked to select 3 answers from the list below, which is presented in rank order:
- Close friend (70%)
- Spouse/life partner (69%)
- Immediate family member (parent/sibling) (65%)
- Rheumatologist (30%)
- Other (please specify) (19%)
- Mental health counsellor (16%)
- Other healthcare team member (16%)
- Online communities (11%)
- Spiritual advisor (4%)
- Patient organization representative (3%)
- Community advisor (like a pastor or minister) (2%)
Seven in 10 respondents living in urban centres get emotional support from a friend. In comparison, 7 in 10 respondents living in rural and small to medium sized communities get emotional support from their spouse.
Findings were significantly different for respondents who identified as black, Indigenous, or a person of colour (BIPOC).
| What is statistical significance? “Statistical significance” refers to a mathematical technique to measure whether the results of a study are likely to be “real”, or simply caused by chance (such as the relationship between race and access to virtual care). When a finding is likely not caused by chance, it is considered statistically significant. |
- Almost 3 times more likely to get emotional support from online communities
- 2 times less likely to get emotional support from their rheumatologist
- 9 times more likely to get emotional support from a community advisor
- 6 times more likely to get emotional support from a patient organization representative

The link between emotional support and mental health
Receiving physical or emotional support is particularly important for people with inflammatory arthritis (IA) who are more likely to experience mental health conditions such as depression, anxiety and “brain fog” than the general population. In fact, those living with rheumatoid arthritis are 17-20% more likely to develop depression.1
A key cause of mental health issues for people diagnosed with arthritis is the pain and disability associated with it. For example, new limitations caused by IA can bring significant changes to one’s life, work, relationships, leading to anxiety and depression. Researchers at the University of Glasgow found that chronic inflammation from IA, which affects joints and organs, such as the eyes, skin, and the brain, may also be related to mental health disorders like depression. “Brain fog” is another symptom of IA – it can create episode of confusion, disorientation and frustration.2

| Work and arthritis |
In terms of sharing information about their disease, a majority of all respondents told their friends or co-workers about their arthritis diagnosis within a few weeks or months after receiving it.
ACE’s Survey also identified statistically significant differences among certain segments of respondents:
- Respondents from rural and small to medium sized communities were 3 times less likely to answer they do not feel comfortable and tell friends or co-workers about their diagnosis compared to respondents from urban centres
- French respondents were 2 times more likely to have not told anyone besides their immediate family members
- English respondents were 3 times more likely to tell friends/co-workers several years after getting their arthritis diagnosis
The Survey asked respondents if they know how to deal with physical limitations caused by their arthritis and that affect their ability to do their job – the majority of respondents answered yes (7 in 10 or 68%), followed by not sure (2 in 10 or 23%) and no (1 in 10 or 8%).
Respondents who identified as BIPOC were more likely to talk about their arthritis diagnosis with their employer than their non-BIPOC counterparts (3 in 4 or 76% compared to 5 in 10 or 55%).
ACE’s Survey also revealed statistical significance related to asking for and receiving job accommodations from an employer:
- BIPOC respondents were 2 times more likely to ask for job accommodations
- 7 in 10 (66%) of non-BIPOC respondents said they have not asked for job accommodations
What respondents told us
ACE probed deeper on the topic of respondents’ experiences and asked them for their perspective on what made them comfortable (or uncomfortable) about sharing their arthritis diagnosis with their employer in their own words:
“Not until I needed surgery. I did not want to be discriminated against in the work place or considered “unable” to do anything or pull my weight. There is nothing worse than other people using your health condition as an excuse for not completing a task which you are collaborating with them on. If the job didn’t get done, it would not be because I have arthritis!”
“Prior bad experiences with employers when they found out. With new job, chose to tell immediate teammates first day, manager at first call after accepting the position. One challenge is having to have the conversation repeatedly as managers and teammates transition.”
The challenges of living with arthritis
Respondents were asked to identify the most challenging things for them to deal with while living with their type of arthritis. They were able to select all that apply from a list – the top 5 answer choices were:
- joint pain (8 in 10 or 78%)
- fatigue (7 in 10 or 75%)
- stiffness (6 in 10 or 61%)
- sleep (5 in 10 or 52%)
- exercise (5 in 10 or 50%)
- more likely to experience challenges in advancing their career (3 in 10 or 33% vs 2 in 10 or 17%)
- 6 times more likely to experience challenges with staying in school (1 in 10 or 12% vs 2%)
- less likely to experience fatigue when compared to the non-BIPOC group (6 in 10 or 58% vs 8 in 10 or 77%)
Getting information on arthritis
The Survey also asked respondents where they usually go to find information about their type of arthritis. The top 5 sources were:
- websites (8 in 10 or 85%)
- members of my health care team (8 in 10 or 77%)
- patient organizations (3 in 10 or 30%)
- other people living with my type of arthritis (3 in 10 or 26%)
- printed pamphlets or guides (2 in 10 or 24%)
ACE’s Survey also asked respondents what arthritis topics they most need information on. Respondents were asked to select 3 choices from the list below presented in rank order:
- Medication treatments (6 in 10 or 56%)
- Non-medication treatments (5 in 10 or 49%)
- Best ways to self-care for my type of arthritis (5 in 10 or 47%)
- My type of arthritis (3 in 10 or 34%)
- Sleep & fatigue (3 in 10 or 30%)
|
In terms of the ability to understand arthritis information, respondents who identified as BIPOC were less likely to find written information about their type of arthritis easy to read and understand (6 in 10 or 56% vs non-BIPOC respondents, at 7 in 10 or 73%). Good health literacy means being able to access, understand, evaluate, communicate and use information related to your health and the health of others to make appropriate health decisions. According to the Public Health Agency of Canada, 60 per cent of seniors are not health literate. |

Respondents and their health care teams
Almost all (99%) of the respondents bring a list of questions or concerns they plan to discuss during their medical appointments. Similarly, 98% were confident about asking questions about their type of arthritis during a medical appointment and 99% were comfortable sharing their health concerns with the health care workers who provide care for their type of arthritis.
Eighty-five per cent of respondents found it “not that difficult” or “not difficult at all” to take action on the information and instructions given to them by their health professional caring for their type of arthritis versus 15% respondents who found it difficult.
What respondents told us
The Survey asked respondents what would help them feel more comfortable asking questions of their health care team members. Here’s what they told us in their own words:
“Written information. Written directions. Guidance on where to go for more information or help. Knowing that I can give them feed back on care directions & get responses. Knowing that there will be follow-up.”
“Generally, it depends on the attitude of the medical professional. If I feel rushed or that they are in a hurry to get to another appointment I won’t ask. Often I don’t have questions until I leave the office and have reflected on the information told to me, so maybe a way to email or contact someone about additional questions afterwards.”

Reaching out to the community
In its Survey, ACE wanted to find out the level of experience respondents had reaching out to members of their arthritis community to get information or share their story.
A surprising 67% of respondents have never asked a patient advocacy organization for help to get the things they need to live with their type of arthritis.
When it comes to sharing their experiences living with their type of arthritis through social media, key findings include:
- French respondents were 4 times less likely to share their experiences on social media
- BIPOC respondents were evenly divided between those who shared their experience on social media (52%) and those who didn’t (48%)
- 70% of non-BIPOC respondents have never shared their experiences on social media compared to 30% who have shared their experiences
- almost 9 in 10 or 86% French respondents (compared to 5 in 10 or 54% English respondents) were not interested in meeting with their elected official
- BIPOC respondents were 2 times more likely to be interested in learning how to contact their elected officials
Two in ten or 19% of respondents have shared their arthritis experiences with mainstream media (community papers, major newspaper, or TV).
What respondents told us
The Survey asked respondents what would make them feel more comfortable sharing their experiences with their type of arthritis through social media? Here’s what they said in their own words:
“Support from the community. Understanding. Compassion.”
“I’ve shared, however only through support groups of those with similar/same diagnosis as they are the most inclusive and supportive communities that I am part of.”
“I wasn’t comfortable at all actually. But I did share about a very specific experience I had on social media to get some traction with our local government about an arthritis program that was closing due to budget cuts.”
Discussion
Self-advocacy is the action of representing their experience, view or interests. For a person living with arthritis, self- advocacy and being an advocate first means being a part of your health care team. It means knowing yourself and speaking up for yourself to make sure that your arthritis care needs are met. A large majority of ACE’s Survey respondents report that they are actively working alongside their healthcare team to choose the best care and treatment for their type of arthritis. These findings suggest respondents know their bodies and understand what’s important to them, what they value and what their priorities are when they consider care and treatment options.
While the term self-advocacy implies advocating for yourself, by yourself, it doesn’t actually mean that you have to do it by yourself. ACE’s Survey respondents reported that many of them bring a friend or family member with them to their meetings with their healthcare team – not just to help take notes but to provide emotional support.
A support system is vital in practicing self-advocacy if you struggle with finding your voice and speaking up for yourself. A more outspoken family member or friend can give you a voice. The top three sources for emotional support cited by Survey respondents were close friend, spouse/partner and immediate family member. The ACE Survey findings also revealed a strong preference with a majority of respondents in terms of who they trust and turn to for information about their arthritis: respondents trusted the advice of their rheumatologist (76%), followed by family physician (8%) and other arthritis specialist and patient organizations (both at 7%).

Advocating at work
Arthritis is the leading cause of work disability in Canada. Arthritis typically occurs during prime working years, between ages 35-50.
ACE’s Survey found that respondents face particular challenges at work. Sixty-six per cent of non-BIPOC respondents said they have not asked for job accommodations. BIPOC respondents were 2 times more likely to experience challenges in advancing their career (33% compared to 17% of non-BIPOC).

Towards a better understanding of how you can advocate at work
Dr. Diane Lacaille of Arthritis Research Canada has conducted studies to determine what workplace factors are closely linked to the risk of a work disability lasting six months or longer.3
Dr. Lacaille found that high physical demand, low job independence (i.e. minimal control over the pace of work and how duties are performed) and poor support from co-workers aggravated arthritis symptoms and accounted for longer absences from work. If no obvious changes need to be made to your work space, your schedule, or your job position, you may decide not to tell people you have a serious type of inflammatory arthritis (IA), like rheumatoid arthritis, at all; there is no legal requirement for you to disclose your IA to your employer or fellow employees. Or perhaps you will begin with telling one or two trusted colleagues, as a way of testing the water and getting practice. It’s up to you. But do bear in mind that people who don’t know you have arthritis won’t know you may need support from time to time. And if at times you need to take frequent breaks or delegate certain tasks, resentment may build if people don’t know the reason and support you.
Flexible work schedules are particularly important for people with IA:
- flexible time allows workers with arthritis to start and finish later, avoiding mornings that are particularly difficult due to increased pain and stiffness;
- split shifts allow shorter consecutive hours of work, allowing to rest;
- right to refuse overtime, especially when disease is not well controlled, without fear of being judged as lacking motivation or commitment.

Resources for arthritis self-advocacy
ACE’s advocacy cycle includes listening carefully to the issues, concerns, and experiences our members share with us. For example, the issue of how the voices of racial minorities are often underrepresented or excluded in health research. We then take that valuable information and create the messages and policy recommendations, find allies and supporters among patients and healthcare providers and deliver our arthritis story or “ask” to elected officials or the media. Here’s what ACE’s advocacy cycle looks like:
- Advocacy Toolkit: A guide to making your voice heard in the public policy process
- Canadian Drug Review, Approval and Reimbursement Process
- ACE’s Election Advocacy
- Self-advocacy Tips
References
| 1 | Nerurker L, Siebert S, et al. Rheumatoid arthritis and depression: an inflammatory perspective. The Lancet Psychiatry. Volume 6, Issue 2, P164-173. October, 2018. DOI: https://doi.org/10.1016/S2215-0366(18)30255-4 |
| 2 | Scherpf A, Kaplan c, et al. A multi-modal MRI study of the central response to inflammation in rheumatoid arthritis. Nature Communications. Volume 9, Issue 1, P2243. June, 2018. DOI https://doi.org/10.1038/s41467-018-04648-0 |
| 3 | Arthritis Research Canada, Dr. Diane Lacaille “Research Interests”: https://www.arthritisresearch.ca/diane-lacaille/ |
Listening to you
We hope you find this information of use. Please tell us what you think by writing to us or emailing us at feedback@jointhealth.org. Through your ongoing and active participation, ACE can make its work more relevant to all Canadians living with arthritis.
Update your email or postal address
Please let us know of any changes by contacting ACE at feedback@jointhealth.org. This will ensure that you continue to receive your free email or print copy of JointHealth™ insight.
Arthritis Consumer Experts (ACE)
Who We Are
Arthritis Consumer Experts (ACE) and its team members acknowledge that they gather and work on the traditional, ancestral and unceded territory of the Coast Salish peoples -ʷməθkʷəy̓əm (Musqueam), Sḵwx̱wú7mesh (Squamish), and Səl̓ílwətaʔ/Selilwitulh (Tsleil-Waututh) Nations.
Arthritis Consumer Experts (ACE) operates as a non-profit and provides free research based education and information to Canadians with arthritis. We help (em)power people living with all forms of arthritis to take control of their disease and to take action in healthcare and research decision making. ACE activities are guided by its members and led by people with arthritis, scientific and medical experts on the ACE Advisory Board. To learn more about ACE, visit www.jointhealth.org
Disclosures
Over the past 12 months, ACE received grants-in-aid from: Arthritis Research Canada, Amgen Canada, Canadian Biosimilars Forum, Canadian Institutes of Health Research, Canadian Rheumatology Association, Eli Lilly Canada, Fresenius Kabi Canada, Gilead Sciences Canada, Hoffman-La Roche Canada Ltd., Knowledge Translation Canada, Merck Canada, Novartis Canada, Pfizer Canada, Sandoz Canada, Sanofi Canada, St. Paul's Hospital (Vancouver), Teva Canada, UCB Canada, and the University of British Columbia.
ACE also received unsolicited donations from its community members (people with arthritis) across Canada.
ACE thanks funders for their support to help the nearly 6 million Canadians living with osteoarthritis, rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis and the many other forms of the disease.
Disclaimer
The material contained on this website is provided for general information only. This website should not be relied on to suggest a course of treatment for a particular individual or as a substitute for consultation with qualified health professionals who are familiar with your individual medical needs. Should you have any healthcare related questions, you should contact your physician. You should never disregard medical advice or delay in seeking it because of something you have read on this or any website.
This site may provide links to other Internet sites only for the convenience of World Wide Web users. ACE is not responsible for the availability or content of these external sites, nor does ACE endorse, warrant or guarantee the products, services or information described or offered at these other Internet sites.
Although the information presented on this website is believed to be accurate at the time it is posted, this website could include inaccuracies, typographical errors or out-of-date information. This website may be changed at any time without prior notice.

