In this issue
- Background
- Survey Methodology
- Who were survey respondents?
- Findings
- Virtual care use before the COVID-19 pandemic
- Virtual care use during the COVID-19 pandemic
- Access to virtual care
- Timeliness of in-person and virtual care
- Arthritis patient level of satisfaction with virtual care services
- Arthritis patient preferences for the future delivery of care
- Participants Thoughts About Virtual Care…
- Conclusion
JointHealth™ insight Published April 2021

 Virtual care—the remote delivery of health care services and information - allows more patients to see their specialists in a timely and convenient way and helps healthcare systems conserve costs.
Virtual care—the remote delivery of health care services and information - allows more patients to see their specialists in a timely and convenient way and helps healthcare systems conserve costs.
During the past year, patients and their healthcare providers have increasingly used virtual care in response to restrictions due to the COVID-19 pandemic.
Arthritis Consumer Experts (ACE) conducted a national survey in English and French from January to February 2021 to understand the arthritis patient community’s experiences and satisfaction using virtual care and if they would like to see virtual care options expanded in the future, post-pandemic.
A key goal of this survey was to identify and address health inequities in virtual care for people living with arthritis. More specifically, to understand how access to virtual care, and experiences using virtual care, differ among demographic groups in the arthritis patient community. This report provides a general summary of respondents’ answers to the survey. In the coming weeks, ACE will be releasing a supplementary report to highlight survey findings related to health inequities in virtual care for people living with arthritis.
Listening to you
We hope you find this information of use. Please tell us what you think by writing to us or emailing us at feedback@jointhealth.org. Through your ongoing and active participation, ACE can make its work more relevant to all Canadians living with arthritis.
Update your email or postal address
Please let us know of any changes by contacting ACE at feedback@jointhealth.org. This will ensure that you continue to receive your free email or print copy of JointHealth™ insight.
Arthritis Consumer Experts (ACE)
Who We Are
Arthritis Consumer Experts (ACE) operates as a non-profit and provides free research based education and information to Canadians with arthritis. We help (em)power people living with all forms of arthritis to take control of their disease and to take action in healthcare and research decision making. ACE activities are guided by its members and led by people with arthritis, scientific and medical experts on the ACE Advisory Board. To learn more about ACE, visit www.jointhealth.org
Disclosures
Over the past 12 months, ACE received grants-in-aid from: Arthritis Research Canada, Amgen Canada, Canadian Biosimilars Forum, Canadian Institutes of Health Research, Canadian Rheumatology Association, Eli Lilly Canada, Fresenius Kabi Canada, Gilead Sciences Canada, Hoffman-La Roche Canada Ltd., Knowledge Translation Canada, Merck Canada, Novartis Canada, Pfizer Canada, Sandoz Canada, Sanofi Canada, St. Paul's Hospital (Vancouver), Teva Canada, UCB Canada, and the University of British Columbia.
ACE also received unsolicited donations from its community members (people with arthritis) across Canada.
ACE thanks funders for their support to help the nearly 6 million Canadians living with osteoarthritis, rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis and the many other forms of the disease.
Disclaimer
The material contained on this website is provided for general information only. This website should not be relied on to suggest a course of treatment for a particular individual or as a substitute for consultation with qualified health professionals who are familiar with your individual medical needs. Should you have any healthcare related questions, you should contact your physician. You should never disregard medical advice or delay in seeking it because of something you have read on this or any website.
This site may provide links to other Internet sites only for the convenience of World Wide Web users. ACE is not responsible for the availability or content of these external sites, nor does ACE endorse, warrant or guarantee the products, services or information described or offered at these other Internet sites.
Although the information presented on this website is believed to be accurate at the time it is posted, this website could include inaccuracies, typographical errors or out-of-date information. This website may be changed at any time without prior notice.


During the past year, patients and their healthcare providers have increasingly used virtual care in response to restrictions due to the COVID-19 pandemic.
Arthritis Consumer Experts (ACE) conducted a national survey in English and French from January to February 2021 to understand the arthritis patient community’s experiences and satisfaction using virtual care and if they would like to see virtual care options expanded in the future, post-pandemic.
A key goal of this survey was to identify and address health inequities in virtual care for people living with arthritis. More specifically, to understand how access to virtual care, and experiences using virtual care, differ among demographic groups in the arthritis patient community. This report provides a general summary of respondents’ answers to the survey. In the coming weeks, ACE will be releasing a supplementary report to highlight survey findings related to health inequities in virtual care for people living with arthritis.
Background

Virtual care has the potential to address what is expected to be a huge increase in the demand for home- and facility-based continuing care as the population ages, particularly those living with complicated chronic diseases like inflammatory arthritis (IA).
For the diagnosis and treatment of complex types of arthritis, it's important that people see a rheumatologist – a specialist specifically trained to treat these diseases. However, many people with IA live in locations where specialists are scarce and/or they experience difficulty traveling (due to symptoms like decreased mobility, imbalance or walking issues). Virtual care – the remote delivery of health care services and information via electronic methods (video conference, smartphones, email, or text) - can address some of these challenges by bringing doctors into patients' homes or nearby clinics.
Survey Methodology
The survey was open from January 20, 2021 through to February 7, 2021 and was open to people living with arthritis. It contained 23 questions and was developed using the online survey platform, Survey Monkey. Respondents required internet access in order to complete the survey.
Thank you from ACE
Thank you to all respondents who took the time to complete our survey. We are extremely grateful for your honest information and thoughtful suggestions.
Who were survey respondents?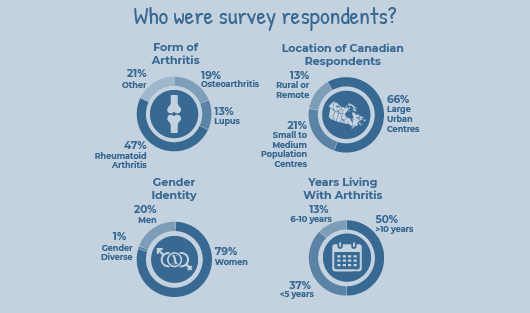 Arthritis Consumer Experts received 253 responses for our community-led survey on virtual care, 173 in English and 80 in French.
Arthritis Consumer Experts received 253 responses for our community-led survey on virtual care, 173 in English and 80 in French.
Findings
Virtual care use before the COVID-19 pandemic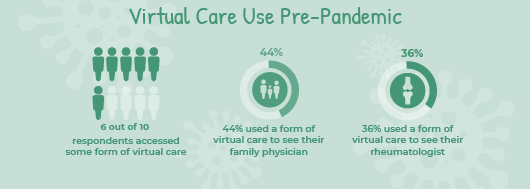
The survey found that nearly all of the respondents were typically seeing their healthcare providers in-person before the start of the pandemic. However, there were a fair number of arthritis patients who, in addition to in-person visits, were also accessing healthcare virtually (by email, telephone and/or video). More specifically, an estimated 6 out of 10 (59%) respondents were already using virtual care to some extent before March 2020, establishing it as an important form of healthcare delivery for many people in the arthritis patient community.
The healthcare providers that patients accessed the most using virtual care pre-COVID-19 pandemic were family doctors (accessed by 44% of respondents) and rheumatologists (36%).
Virtual care use during the COVID-19 pandemic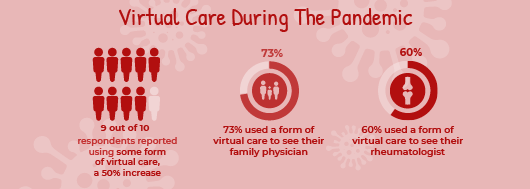
Survey findings show that there has been a substantial shift in the way people living with arthritis have accessed care since March 2020. Arthritis patients have increasingly relied on virtual care during the pandemic, although they have also been accessing healthcare in more than one way, including a mix of both in-person and virtual formats.
Since March 2020, there has been a 20 per cent total decline in the number of people who have had any in-person visits with their healthcare providers. As in-person visits have declined, virtual care use has significantly increased.
In fact, almost 9 out of 10 (88%) respondents have accessed virtual care during the pandemic. This represents a 50% total increase in respondents use of virtual care since the start of the pandemic.
Telephone (73%) was the most common form of virtual care that respondents reported using. Video conferencing (28%) and email (24%) were the next most common forms used by arthritis patients.
Access to virtual care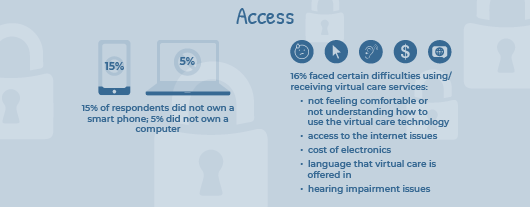
Virtual care is commonly delivered through a patient’s smartphone or computer as it often involves emailing, phone calls and/ or videoconferencing with healthcare providers. Fifteen per cent (15%) of survey respondents did not own a smart phone and just over 5% of respondents did not own a computer. For those who did not own either a smart phone or computer, the majority also did not have access to these devices in a shared format (such as access to a smartphone or computer through their household, a community centre or library). It is important to note that because this survey was administered online, it may have restricted people who do not own a smart phone or computer from participating. The true number of people living with arthritis who do not own smartphones or computers is certainly much higher.
While the majority of respondents did not report any difficulties using virtual care services, 16% did report facing difficulties of some kind. The most common difficulty identified was not feeling comfortable or not understanding how to use the virtual care technology offered by their healthcare professional. The significance of this issue for some people living with arthritis, and how it impacts their use of virtual care services, is illustrated in this quote from a respondent:
“I live on my own and do not know how to use electronics. I rely on family members to be at my resident [home] and on the telephone visit with me”.
The second most common difficulty that arthritis patients reported in relation to using virtual care was access to the internet, followed by the cost of electronics, and, lastly, the language that virtual care is offered in (i.e., lack of translation services). Respondents also commented that because they are hearing impaired, it is challenging to do video conference and telephone calls.
Timeliness of in-person and virtual care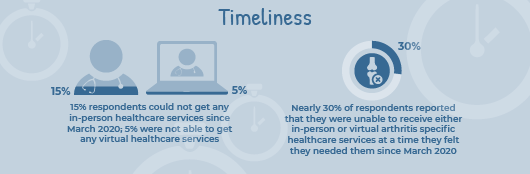
Despite the mix of in-person and virtual care services being used, it appears that many arthritis patients are still falling through the cracks and have not been able to receive care in a timely manner during the pandemic. For example, almost 3 out of 10 (27%) respondents reported that they were unable to receive arthritis specific healthcare services in-person at a time they felt they needed them since March 2020. Thirty-two per cent of respondents reported that they were unable to receive arthritis specific healthcare services virtually at a time they felt they needed them since March 2020.
Three in 20 (15%) reported that they were unable to get any arthritis healthcare services in person since March 2020 while 1 in 20 (5%) were not able to get any arthritis healthcare services virtually.
Arthritis patient level of satisfaction with virtual care services
A majority of arthritis patients were satisfied sharing their health concerns and getting advice from health care providers through virtual care. Fifty-eight per cent were either very satisfied or satisfied, and 27% were somewhat satisfied. 7.5% reported that they were dissatisfied, and 3% were “very dissatisfied”. Four per cent did not answer this question as they did not finish the survey.
When asked what they liked about virtual healthcare services, if they had accessed them since March 2020, most respondents (7 in 10, 70%) selected:
One in 5 (21%) arthritis patients reported they liked virtual care because it allowed them to see their healthcare providers more quickly. A smaller portion of respondents (1 in 10 or just under 10%) reported they felt more comfortable sharing their health concerns virtually compared to in-person.
Survey respondents also identified a number of elements they like about in-person appointments that cannot be replicated in a virtual setting. When asked to select from multiple answers about what they liked about in-person appointments with their healthcare team, the most popular answers were:
Arthritis patient preferences for the future delivery of care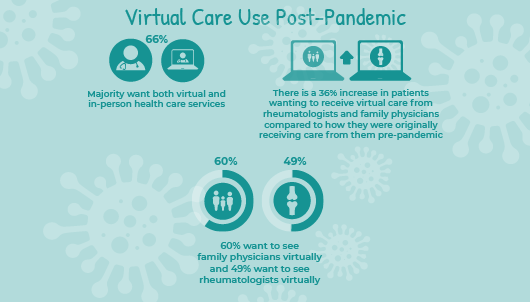
The survey found that the majority of arthritis patients would like the option of seeing healthcare providers both virtually and in-person.
When asked how they would like to access healthcare in the future (respondents could select more than one way of accessing care), nearly all respondents (96%) wanted to be able to see healthcare providers in-person post-pandemic. Sixty-six per cent (66%) of arthritis patients reported they would also like the option of seeing healthcare providers virtually when the pandemic is over.
Three out of 4 respondents stated that it was either very important (30%), important (21%) or somewhat important (24%) to continue to have access to virtual health care services after the pandemic ends.
Arthritis patients are particularly interested in having greater access to virtual care appointments with key providers (like rheumatologists and family physicians) than they were originally receiving pre-pandemic. For example, when it comes to family physicians, there is a 36% increase in people wanting to receive virtual care from them compared to how they were originally receiving care from them pre-pandemic. For rheumatologists, there is also an increase of 36%.
Many arthritis patients who provided comments in the “other (please specify)” answer option of the survey expressed their desire for a mix of in-person and virtual care services in the future, noting that virtual care is valuable to supplement, but not replace, in-person appointments. Some of these comments are highlighted below:
Participants Thoughts About Virtual Care…
“A mix of virtual and in-person. I'd like to have an option.”
“Video conference with my rheumatologist is good as long as I am well. It is less tiring than going to the office and more comfortable.”
“I would really like a mix of care - in person for more urgent things and when I want my doctor to see a swollen joint or something, and then virtual care for stuff I need that doesn't really warrant a visit like a prescription refill, blood test requisition etc.”
Conclusion
Findings from our community-led research have shown that virtual care has been an important form of healthcare delivery for many people living with arthritis before the COVID-19 pandemic and increasingly more, since March 2020, when patients have been relying on virtual care to a much greater degree. Arthritis patients would like to continue having the option to access virtual care even when the pandemic is over. They would like greater access to virtual care than they were originally receiving pre-pandemic, specifically, connections with key healthcare providers like family doctors and rheumatologists. A majority of arthritis patients reported their preference for a mix of in-person and virtual care services, with a preference of in-person for more complex examinations such as joint counts, and virtual consults to augment care (e.g. in-between visits or to support patient self-care).
Overall, arthritis patients’ satisfaction with virtual care was high and appeared to be equal to standard face-to-face encounters with rheumatologists or family physicians. However, the survey identified a number of difficulties that arthritis patients are experiencing when it comes to accessing virtual care and receiving arthritis specific health services in a timely manner. These challenges (access to the internet, cost of electronics, lack of translation services) act as barriers to meaningfully accessing and benefitting from virtual care. With these challenges in mind and an arthritis patient preference for a mix use of in-person and virtual care, for the best outcomes today, it should be a shared decision with patients as to whom and when is it most appropriate to provide virtual care. Moving forward, more research must be done to better understand patient preferences for virtual care as it may not be acceptable for all patients.
Our next issue of JointHealth™ insight will take an in-depth look at the health inequity findings from Arthritis Consumer Experts’ virtual care survey, where we examine which groups in the arthritis patient community are being particularly impacted by these challenges.

Virtual care has the potential to address what is expected to be a huge increase in the demand for home- and facility-based continuing care as the population ages, particularly those living with complicated chronic diseases like inflammatory arthritis (IA).
For the diagnosis and treatment of complex types of arthritis, it's important that people see a rheumatologist – a specialist specifically trained to treat these diseases. However, many people with IA live in locations where specialists are scarce and/or they experience difficulty traveling (due to symptoms like decreased mobility, imbalance or walking issues). Virtual care – the remote delivery of health care services and information via electronic methods (video conference, smartphones, email, or text) - can address some of these challenges by bringing doctors into patients' homes or nearby clinics.
Survey Methodology
The survey was open from January 20, 2021 through to February 7, 2021 and was open to people living with arthritis. It contained 23 questions and was developed using the online survey platform, Survey Monkey. Respondents required internet access in order to complete the survey.
Thank you from ACE
Thank you to all respondents who took the time to complete our survey. We are extremely grateful for your honest information and thoughtful suggestions.
Who were survey respondents?
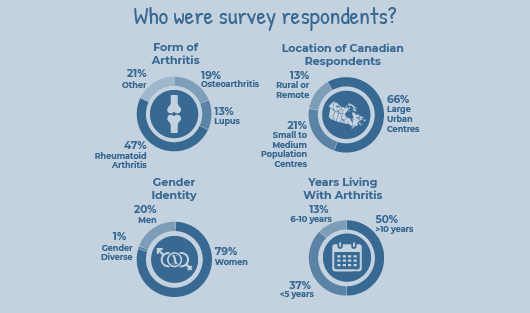 Arthritis Consumer Experts received 253 responses for our community-led survey on virtual care, 173 in English and 80 in French.
Arthritis Consumer Experts received 253 responses for our community-led survey on virtual care, 173 in English and 80 in French.
- Respondents were patients living with different forms of arthritis, including osteoarthritis, rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis, lupus, juvenile idiopathic arthritis, fibromyalgia, Sjögren’s syndrome, scleroderma, vasculitis, adult-onset Still’s disease and uveitis. The three most common forms of arthritis among respondents were rheumatoid arthritis (accounting for almost half of the respondents), osteoarthritis (2 in 10 or 19%), and lupus (1 in 10 or 13%)
- Nearly half of respondents have been living with arthritis for over 10 years, while 1 in 10 (13%) have been living with arthritis between 6-10 years and 2 in 5 (37%) have been living with arthritis for 5 years or less.
- The majority (9 in 10 or 90%) of respondents were Canadian residents. One in 10 of the respondents were international, including patients from the U.S., England, Ireland, Sweden, Scotland, Australia and Africa. Sixty-six per cent of respondents reported living in large urban centres, 21% in small to medium sized population centres, and 13% from rural or remote communities.
- In terms of gender, 4 in 5 (79%) of respondents were women, 1 in 5 (20%) were men and approximately 1% identified as gender diverse.
Findings
Virtual care use before the COVID-19 pandemic
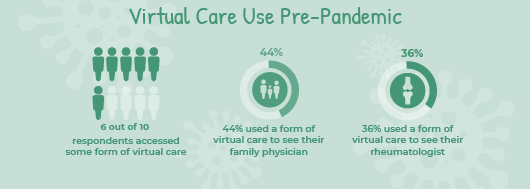
The survey found that nearly all of the respondents were typically seeing their healthcare providers in-person before the start of the pandemic. However, there were a fair number of arthritis patients who, in addition to in-person visits, were also accessing healthcare virtually (by email, telephone and/or video). More specifically, an estimated 6 out of 10 (59%) respondents were already using virtual care to some extent before March 2020, establishing it as an important form of healthcare delivery for many people in the arthritis patient community.
The healthcare providers that patients accessed the most using virtual care pre-COVID-19 pandemic were family doctors (accessed by 44% of respondents) and rheumatologists (36%).
Virtual care use during the COVID-19 pandemic
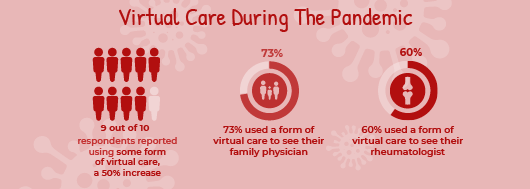
Survey findings show that there has been a substantial shift in the way people living with arthritis have accessed care since March 2020. Arthritis patients have increasingly relied on virtual care during the pandemic, although they have also been accessing healthcare in more than one way, including a mix of both in-person and virtual formats.
Since March 2020, there has been a 20 per cent total decline in the number of people who have had any in-person visits with their healthcare providers. As in-person visits have declined, virtual care use has significantly increased.
In fact, almost 9 out of 10 (88%) respondents have accessed virtual care during the pandemic. This represents a 50% total increase in respondents use of virtual care since the start of the pandemic.
Telephone (73%) was the most common form of virtual care that respondents reported using. Video conferencing (28%) and email (24%) were the next most common forms used by arthritis patients.
Access to virtual care
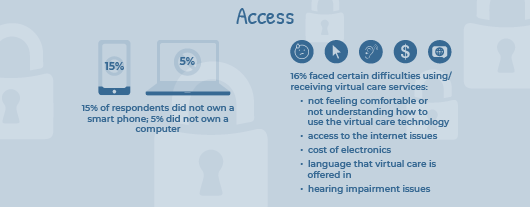
Virtual care is commonly delivered through a patient’s smartphone or computer as it often involves emailing, phone calls and/ or videoconferencing with healthcare providers. Fifteen per cent (15%) of survey respondents did not own a smart phone and just over 5% of respondents did not own a computer. For those who did not own either a smart phone or computer, the majority also did not have access to these devices in a shared format (such as access to a smartphone or computer through their household, a community centre or library). It is important to note that because this survey was administered online, it may have restricted people who do not own a smart phone or computer from participating. The true number of people living with arthritis who do not own smartphones or computers is certainly much higher.
While the majority of respondents did not report any difficulties using virtual care services, 16% did report facing difficulties of some kind. The most common difficulty identified was not feeling comfortable or not understanding how to use the virtual care technology offered by their healthcare professional. The significance of this issue for some people living with arthritis, and how it impacts their use of virtual care services, is illustrated in this quote from a respondent:
“I live on my own and do not know how to use electronics. I rely on family members to be at my resident [home] and on the telephone visit with me”.
The second most common difficulty that arthritis patients reported in relation to using virtual care was access to the internet, followed by the cost of electronics, and, lastly, the language that virtual care is offered in (i.e., lack of translation services). Respondents also commented that because they are hearing impaired, it is challenging to do video conference and telephone calls.
Timeliness of in-person and virtual care
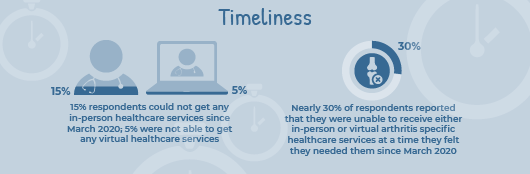
Despite the mix of in-person and virtual care services being used, it appears that many arthritis patients are still falling through the cracks and have not been able to receive care in a timely manner during the pandemic. For example, almost 3 out of 10 (27%) respondents reported that they were unable to receive arthritis specific healthcare services in-person at a time they felt they needed them since March 2020. Thirty-two per cent of respondents reported that they were unable to receive arthritis specific healthcare services virtually at a time they felt they needed them since March 2020.
Three in 20 (15%) reported that they were unable to get any arthritis healthcare services in person since March 2020 while 1 in 20 (5%) were not able to get any arthritis healthcare services virtually.
Arthritis patient level of satisfaction with virtual care services

A majority of arthritis patients were satisfied sharing their health concerns and getting advice from health care providers through virtual care. Fifty-eight per cent were either very satisfied or satisfied, and 27% were somewhat satisfied. 7.5% reported that they were dissatisfied, and 3% were “very dissatisfied”. Four per cent did not answer this question as they did not finish the survey.
When asked what they liked about virtual healthcare services, if they had accessed them since March 2020, most respondents (7 in 10, 70%) selected:
- They did not have to travel to appointments, and;
- They were not at risk of getting COVID-19 due to an in-person appointment.
One in 5 (21%) arthritis patients reported they liked virtual care because it allowed them to see their healthcare providers more quickly. A smaller portion of respondents (1 in 10 or just under 10%) reported they felt more comfortable sharing their health concerns virtually compared to in-person.
Survey respondents also identified a number of elements they like about in-person appointments that cannot be replicated in a virtual setting. When asked to select from multiple answers about what they liked about in-person appointments with their healthcare team, the most popular answers were:
- Full or partial joint examination (selected by 79% of respondents), and;
- Face-to-face interaction with immediate feedback from my healthcare team (selected by 75% of respondents).
Arthritis patient preferences for the future delivery of care
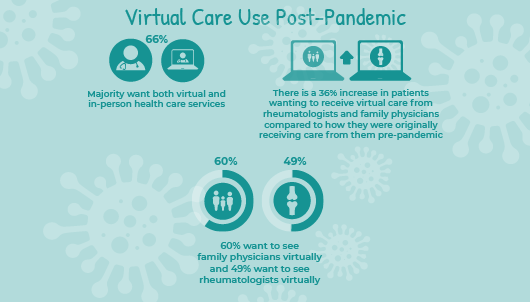
The survey found that the majority of arthritis patients would like the option of seeing healthcare providers both virtually and in-person.
When asked how they would like to access healthcare in the future (respondents could select more than one way of accessing care), nearly all respondents (96%) wanted to be able to see healthcare providers in-person post-pandemic. Sixty-six per cent (66%) of arthritis patients reported they would also like the option of seeing healthcare providers virtually when the pandemic is over.
Three out of 4 respondents stated that it was either very important (30%), important (21%) or somewhat important (24%) to continue to have access to virtual health care services after the pandemic ends.
Arthritis patients are particularly interested in having greater access to virtual care appointments with key providers (like rheumatologists and family physicians) than they were originally receiving pre-pandemic. For example, when it comes to family physicians, there is a 36% increase in people wanting to receive virtual care from them compared to how they were originally receiving care from them pre-pandemic. For rheumatologists, there is also an increase of 36%.
Many arthritis patients who provided comments in the “other (please specify)” answer option of the survey expressed their desire for a mix of in-person and virtual care services in the future, noting that virtual care is valuable to supplement, but not replace, in-person appointments. Some of these comments are highlighted below:
Participants Thoughts About Virtual Care…

“A mix of virtual and in-person. I'd like to have an option.”
“In person if situation needs physical assessment, otherwise virtual appointments would be good.”
“Video conference with my rheumatologist is good as long as I am well. It is less tiring than going to the office and more comfortable.”
“I would like a combo of in person and telephone, video, text. It’s very convenient to simply call my GP and have a video meeting with my rheumatologists.”
“I would really like a mix of care - in person for more urgent things and when I want my doctor to see a swollen joint or something, and then virtual care for stuff I need that doesn't really warrant a visit like a prescription refill, blood test requisition etc.”
Conclusion
Findings from our community-led research have shown that virtual care has been an important form of healthcare delivery for many people living with arthritis before the COVID-19 pandemic and increasingly more, since March 2020, when patients have been relying on virtual care to a much greater degree. Arthritis patients would like to continue having the option to access virtual care even when the pandemic is over. They would like greater access to virtual care than they were originally receiving pre-pandemic, specifically, connections with key healthcare providers like family doctors and rheumatologists. A majority of arthritis patients reported their preference for a mix of in-person and virtual care services, with a preference of in-person for more complex examinations such as joint counts, and virtual consults to augment care (e.g. in-between visits or to support patient self-care).
Overall, arthritis patients’ satisfaction with virtual care was high and appeared to be equal to standard face-to-face encounters with rheumatologists or family physicians. However, the survey identified a number of difficulties that arthritis patients are experiencing when it comes to accessing virtual care and receiving arthritis specific health services in a timely manner. These challenges (access to the internet, cost of electronics, lack of translation services) act as barriers to meaningfully accessing and benefitting from virtual care. With these challenges in mind and an arthritis patient preference for a mix use of in-person and virtual care, for the best outcomes today, it should be a shared decision with patients as to whom and when is it most appropriate to provide virtual care. Moving forward, more research must be done to better understand patient preferences for virtual care as it may not be acceptable for all patients.
Our next issue of JointHealth™ insight will take an in-depth look at the health inequity findings from Arthritis Consumer Experts’ virtual care survey, where we examine which groups in the arthritis patient community are being particularly impacted by these challenges.
| Thank you again to the people who took time to participate in this important community-led research, and to our community partners who helped promote the survey through their communication channels. |
Listening to you
We hope you find this information of use. Please tell us what you think by writing to us or emailing us at feedback@jointhealth.org. Through your ongoing and active participation, ACE can make its work more relevant to all Canadians living with arthritis.
Update your email or postal address
Please let us know of any changes by contacting ACE at feedback@jointhealth.org. This will ensure that you continue to receive your free email or print copy of JointHealth™ insight.
Arthritis Consumer Experts (ACE)
Who We Are
Arthritis Consumer Experts (ACE) operates as a non-profit and provides free research based education and information to Canadians with arthritis. We help (em)power people living with all forms of arthritis to take control of their disease and to take action in healthcare and research decision making. ACE activities are guided by its members and led by people with arthritis, scientific and medical experts on the ACE Advisory Board. To learn more about ACE, visit www.jointhealth.org
Disclosures
Over the past 12 months, ACE received grants-in-aid from: Arthritis Research Canada, Amgen Canada, Canadian Biosimilars Forum, Canadian Institutes of Health Research, Canadian Rheumatology Association, Eli Lilly Canada, Fresenius Kabi Canada, Gilead Sciences Canada, Hoffman-La Roche Canada Ltd., Knowledge Translation Canada, Merck Canada, Novartis Canada, Pfizer Canada, Sandoz Canada, Sanofi Canada, St. Paul's Hospital (Vancouver), Teva Canada, UCB Canada, and the University of British Columbia.
ACE also received unsolicited donations from its community members (people with arthritis) across Canada.
ACE thanks funders for their support to help the nearly 6 million Canadians living with osteoarthritis, rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis and the many other forms of the disease.
Disclaimer
The material contained on this website is provided for general information only. This website should not be relied on to suggest a course of treatment for a particular individual or as a substitute for consultation with qualified health professionals who are familiar with your individual medical needs. Should you have any healthcare related questions, you should contact your physician. You should never disregard medical advice or delay in seeking it because of something you have read on this or any website.
This site may provide links to other Internet sites only for the convenience of World Wide Web users. ACE is not responsible for the availability or content of these external sites, nor does ACE endorse, warrant or guarantee the products, services or information described or offered at these other Internet sites.
Although the information presented on this website is believed to be accurate at the time it is posted, this website could include inaccuracies, typographical errors or out-of-date information. This website may be changed at any time without prior notice.

