In this issue
- A closer look at the ethical and societal questions surrounding the COVID-19 vaccine
- Who gets vaccinated first?
- But after essential groups, who comes next?
- Immunity passports?
- What happens if you suffer side effects?
- Can you choose which vaccine you want?
- Can you refuse the vaccine?
- How to make this holiday fun, safe and healthy
JointHealth™ insight Published December 2020


As an incredibly challenging 2020 comes to a close, Arthritis Consumer Experts (ACE) looks to 2021 with confidence and optimism for the arthritis patient community. In this issue of JointHealth™ insight, we take a closer look at the development and distribution of the COVID-19 vaccine and provide tips for celebrating the holidays this season.

Listening to you
We hope you find this information of use. Please tell us what you think by writing to us or emailing us at feedback@jointhealth.org. Through your ongoing and active participation, ACE can make its work more relevant to all Canadians living with arthritis.
Update your email or postal address
Please let us know of any changes by contacting ACE at feedback@jointhealth.org. This will ensure that you continue to receive your free email or print copy of JointHealth™ insight.
Arthritis Consumer Experts (ACE)
Who We Are
Arthritis Consumer Experts (ACE) operates as a non-profit and provides free research based education and information to Canadians with arthritis. We help (em)power people living with all forms of arthritis to take control of their disease and to take action in healthcare and research decision making. ACE activities are guided by its members and led by people with arthritis, scientific and medical experts on the ACE Advisory Board. To learn more about ACE, visit www.jointhealth.org
Disclosures
Over the past 12 months, ACE received grants- in-aid from: Arthritis Research Canada, Amgen Canada, Canadian Institutes of Health Research, Canadian Rheumatology Association, Eli Lilly Canada, Hoffman-La Roche Canada Ltd., Knowledge Translation Canada, Merck Canada, Novartis Canada, Pfizer Canada, Sandoz Canada, Sanofi Canada, St. Paul’s Hospital (Vancouver), UCB Canada, and the University of British Columbia.
ACE also received unsolicited donations from its community members (people with arthritis) across Canada.
ACE thanks funders for their support to help the nearly 6 million Canadians living with osteoarthritis, rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis and the many other forms of the disease.
Disclaimer
The material contained on this website is provided for general information only. This website should not be relied on to suggest a course of treatment for a particular individual or as a substitute for consultation with qualified health professionals who are familiar with your individual medical needs. Should you have any healthcare related questions, you should contact your physician. You should never disregard medical advice or delay in seeking it because of something you have read on this or any website.
This site may provide links to other Internet sites only for the convenience of World Wide Web users. ACE is not responsible for the availability or content of these external sites, nor does ACE endorse, warrant or guarantee the products, services or information described or offered at these other Internet sites.
Although the information presented on this website is believed to be accurate at the time it is posted, this website could include inaccuracies, typographical errors or out-of-date information. This website may be changed at any time without prior notice.



A closer look at the ethical and societal questions surrounding the COVID-19 vaccine
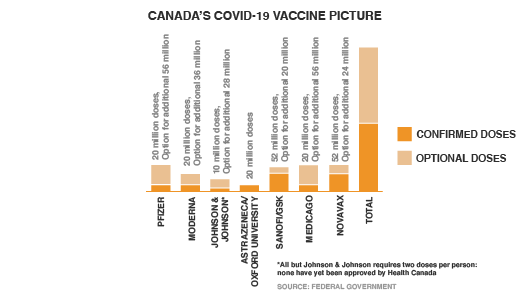
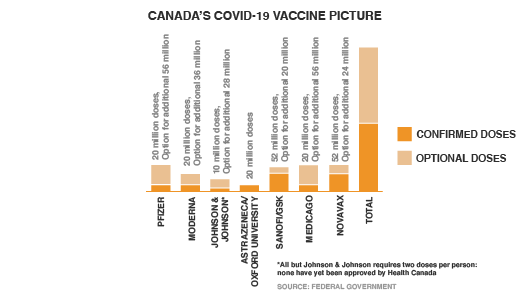
As the federal government makes plans for the procurement and distribution of COVID-19 vaccines, signing contracts with seven potential manufacturers, it is predicting the majority of the six million doses will arrive in the country between December 2020 and the first quarter of 2021. The government anticipates covering the vast majority of the population by the end of 2021.
 When the first doses of COVID-19 vaccines finally do arrive in Canada, we will need to grapple with a series of difficult questions that government officials, public health experts and ethicists have been trying to answer. Which groups should get vaccinated after those most vulnerable? Are certain vaccines more effective with certain populations versus others? How long will it take for everyone to get their shot? And what happens if a person refuses to get vaccinated?
When the first doses of COVID-19 vaccines finally do arrive in Canada, we will need to grapple with a series of difficult questions that government officials, public health experts and ethicists have been trying to answer. Which groups should get vaccinated after those most vulnerable? Are certain vaccines more effective with certain populations versus others? How long will it take for everyone to get their shot? And what happens if a person refuses to get vaccinated?
The clock is ticking to address these questions. Pfizer’s vaccine candidate, which is 95-per-cent effective according to the company’s preliminary results, was approved by Health Canada on December 9, 2020, a key step toward launching the largest inoculation campaign in Canada’s history.
Canadian provinces and territories, which are responsible for the delivery of vaccines to residents, are waiting for more clarity from the federal government as they scramble to develop a province-wide vaccination strategy. Most provinces have stated they anticipate having a vaccination strategy completed by the start of 2021.1
Without a clearly articulated, transparent guideline for the “efficient, effective, equitable allocation of the COVID-19 vaccine,” the uncertainty around the roll-out is making people very anxious, including many ACE members across the country who are vulnerable and high-risk patients living with inflammatory arthritis.

Who gets vaccinated first?
Canadian federal health authorities have not released a comprehensive list of what order the vaccine will be delivered. The distribution model could become complicated if dosages of the vaccine are available in phases – not all at once – forcing government officials to prioritize who first gets the vaccine.
For now, four key groups have been given priority to receive the vaccine, according to recommendations from the National Advisory Committee on Immunization. Those groups include those at risk of severe illness and death (such as the elderly or those with pre-existing conditions), essential workers most likely to transmit the disease (such as health-care workers), those at risk who live in communities that could suffer disproportionate consequences (such as isolated Indigenous communities), and other workers providing services that contribute to “the functioning of society.” People who are unable to work remotely and are at risk of exposure, like police, firefighters and grocery store staff, are also among the key groups in NACI’s recommendations. There will also be groups who won’t be able to get a vaccine early on, due to the lack of research into the potential impacts on them, such as children and women who are pregnant.
The NACI purposefully left the definitions broad so that policy makers at provinces and territories responsible for strategizing vaccine roll-outs could refine the prioritizations based on their own regional demographics.

But after essential groups, who comes next?
Canada’s chief public health officer Dr. Theresa Tam said that according to what the science suggests about who is most at risk from COVID-19, the initial round of vaccines should go to those in high-risk situations such as hospitals and care homes. The next batch, she added, should be done by age, with the oldest at the front of the line: “We know that underlying medical conditions put people at high risk but when we actually analyze all the different underlying medical conditions, and their age, it still comes out that the age is in fact the most important where you look at severe illness and mortality.”3
Some provinces, like Alberta, have floated the idea, the vaccines should be distributed by population. Governments will also be listening carefully to the pleas from employers whose businesses have been severely disrupted due to COVID-19 to ensure their employees are prioritized to get vaccinated. A recent Statistics Canada survey from mid-September to late October found that five per cent of businesses were actively considering bankruptcy or closure this fall. Anxieties are running highest among the arts, entertainment and hospitality industries, with nearly 30 per cent worried they’ll need to resort to layoffs, bankruptcy or closure within six months.
There are other important ethical and societal consideration on who should be prioritized and is related to how disproportionately COVID-19 has affected ethnic and low-income Canadians. As ACE has reported throughout the pandemic, researchers have found Black, South Asian and Indigenous Canadians are far more likely than white Canadians to have multiple medical conditions putting them at higher risk of severe outcomes, including mortality, from COVID-19.
In our Fall issue of JointHealth™ insight, we also looked at the significantly higher percentage of COVID-19 cases happening in visible minorities as well as low-income households.
According to Prime Minister Trudeau reporting after a first minister’s call on November 12, 2020, there seems to be a consensus among federal, provincial and territory government that we should all agree across the country on what the prioritization list looks like and make sure that it is applied fairly right across the country.4
Given the health inequities that historically exist in Canada (see ACE’s Arthritis Medications Report Card), whatever happens when Canadians line up to be vaccinated, we can anticipate there will potentially be a period of time in 2021 when the limited supply of vaccines will create a society of haves and have-nots.
Immunity passports?
The idea of “immunity passports” was floated early on in the pandemic as some governments expressed optimism that individuals who’d recovered from COVID-19 and tested positive for virus-fighting antibodies could be given greater freedoms to travel or return to work. However, the World Health Organization dismissed the idea, saying there wasn’t enough evidence yet on the effectiveness or longevity of immunity through antibodies.
Vaccines may give new attention to the notion of “immunity passports” -- a possibility that public health experts say needs to be handled thoughtfully. For example, these experts describe scenarios where employers and regulators use people’s immune status to selectively grant them access to employment and travel.
What happens if you suffer side effects?
As Canada gets closer to authorizing more COVID-19 vaccines, many ACE members have been asking what it will feel like to get it? Is it going to be like the flu vaccine? Will it be more painful? And what about side-effects?
The two front-runners for getting an emergency use authorization from Health Canada - Pfizer and Moderna -- use new mRNA technology. These vaccines require two doses: one to prime the body, and then a few weeks later, a second shot to boost the response. Study results show that Pfizer and Moderna’s vaccines are each in the range of 95% effective. But because the technology is so new for a vaccine, it has raised many questions and some public concerns.
All COVID-19 vaccines currently being studied are tested for both their effectiveness and safety. Before reaching the general public, Health Canada needs to authorize that the vaccine is safe enough for public use. Even so, there’s a chance that some individuals could suffer long-term side effects from a COVID-19 vaccine.
In the rare event that someone suffers negative side effects of the vaccine, some public health experts believe they should be financially compensated. More than 20 countries, including all other G7 countries, have programs that compensate individuals injured by vaccines. The Government of Canada announced on December 10, 2020 that it will be introducing an injury support program for all vaccines approved by Health Canada, including those developed for COVID-19. As stated by the Public Health Agency of Canada: ,“ building on the model in place in Québec for over 30 years, the program will ensure that all Canadians have to have fair access to support in the rare event that they experience an adverse reaction to a vaccine”.
Can you choose which vaccine you want?
With seven vaccine candidates in the race to be authorized after Pfizer’s, Canada will have several different vaccines on the market in 2021. However, experts say that there is no health benefit to receiving more than one type of vaccine. As for personal choice, it’s unlikely that Canadians will have the option to choose which vaccine they want. Instead, it will depend upon the agreement the provinces and territories reach with the federal government on how many doses of a particular vaccine they receive. The primary issue for these jurisdictions as the vaccines arrive in Canada will not be choice but prioritizing the population segments to receive the vaccine.
 Can you refuse the vaccine?
Can you refuse the vaccine?
Over the course of the pandemic since the outbreak in March 2020, vaccine confidence has declined and a consistent portion of Canadians remain undecided about whether to get vaccinated.
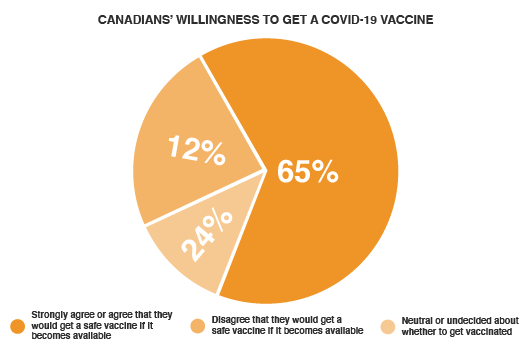
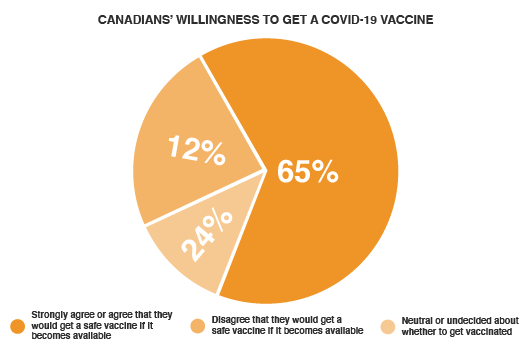
According to Government of Canada surveys, 65% of respondents strongly agree or agree that they would get a safe vaccine if it becomes available and only 43% think that vaccines are completely safe. Twenty-four per cent of Canadians are neutral or undecided about whether to get vaccinated. Concerns around a lack of research and testing, the safety/effectiveness of a vaccine, and the newness of the vaccine were the most prevalent reasons for not wanting to receive a safe vaccine once developed.5
It’s impossible for anyone to be forced to take the COVID-19 vaccine once it’s available. But there could be real-life consequences to refusal. For instance, individuals who aren’t vaccinated may miss out on returning to the workplace or could face other restrictions involving group gatherings.
 The distrust people have in the COVID-19 vaccine is part of a long-standing anti-vaccination movement in North America, but also a product of the “infodemic” that has coincided with the pandemic. In an August JointHealth™ insight, ACE focused on this infodemic as defined by the World Health Organization as “an overabundance of information, some accurate and some not—that makes it hard for people to find trustworthy sources and reliable guidance when they need it.”
The distrust people have in the COVID-19 vaccine is part of a long-standing anti-vaccination movement in North America, but also a product of the “infodemic” that has coincided with the pandemic. In an August JointHealth™ insight, ACE focused on this infodemic as defined by the World Health Organization as “an overabundance of information, some accurate and some not—that makes it hard for people to find trustworthy sources and reliable guidance when they need it.”
Even when people have access to high-quality information on the vaccine, misinformation about it continues to spread further and faster and adds complexity to our trust and acceptance of its safety and efficacy. We have seen a similar phenomenon over the past year with the decision to not wear a mask as a means to slow the spread of the virus, which has had less to do with the pandemic than a distrust in authorities and science.
Governments, healthcare leaders and the digital platforms where people find the misinformation must address the “fake news” that undermines our shared ability to vaccinate against COVID-19 and build trust in the communities where vaccine misinformation has taken root.
An example of that effort occurred on December 3, 2020, when Facebook announced it would remove posts that contain claims about COVID-19 vaccines that have been discredited or contradicted by health groups including the World Health Organization, the United States Food and Drug Administration and the Centers for Disease Control and Prevention.6
The World Health Organization has prepared a guide – “How to respond to a vaccine denier” - to help organizations and individuals respond to vaccination misinformation. Click here to learn more.



As the federal government makes plans for the procurement and distribution of COVID-19 vaccines, signing contracts with seven potential manufacturers, it is predicting the majority of the six million doses will arrive in the country between December 2020 and the first quarter of 2021. The government anticipates covering the vast majority of the population by the end of 2021.
 When the first doses of COVID-19 vaccines finally do arrive in Canada, we will need to grapple with a series of difficult questions that government officials, public health experts and ethicists have been trying to answer. Which groups should get vaccinated after those most vulnerable? Are certain vaccines more effective with certain populations versus others? How long will it take for everyone to get their shot? And what happens if a person refuses to get vaccinated?
When the first doses of COVID-19 vaccines finally do arrive in Canada, we will need to grapple with a series of difficult questions that government officials, public health experts and ethicists have been trying to answer. Which groups should get vaccinated after those most vulnerable? Are certain vaccines more effective with certain populations versus others? How long will it take for everyone to get their shot? And what happens if a person refuses to get vaccinated?The clock is ticking to address these questions. Pfizer’s vaccine candidate, which is 95-per-cent effective according to the company’s preliminary results, was approved by Health Canada on December 9, 2020, a key step toward launching the largest inoculation campaign in Canada’s history.
Canadian provinces and territories, which are responsible for the delivery of vaccines to residents, are waiting for more clarity from the federal government as they scramble to develop a province-wide vaccination strategy. Most provinces have stated they anticipate having a vaccination strategy completed by the start of 2021.1
Without a clearly articulated, transparent guideline for the “efficient, effective, equitable allocation of the COVID-19 vaccine,” the uncertainty around the roll-out is making people very anxious, including many ACE members across the country who are vulnerable and high-risk patients living with inflammatory arthritis.

Who gets vaccinated first?
Canadian federal health authorities have not released a comprehensive list of what order the vaccine will be delivered. The distribution model could become complicated if dosages of the vaccine are available in phases – not all at once – forcing government officials to prioritize who first gets the vaccine.
For now, four key groups have been given priority to receive the vaccine, according to recommendations from the National Advisory Committee on Immunization. Those groups include those at risk of severe illness and death (such as the elderly or those with pre-existing conditions), essential workers most likely to transmit the disease (such as health-care workers), those at risk who live in communities that could suffer disproportionate consequences (such as isolated Indigenous communities), and other workers providing services that contribute to “the functioning of society.” People who are unable to work remotely and are at risk of exposure, like police, firefighters and grocery store staff, are also among the key groups in NACI’s recommendations. There will also be groups who won’t be able to get a vaccine early on, due to the lack of research into the potential impacts on them, such as children and women who are pregnant.
The NACI purposefully left the definitions broad so that policy makers at provinces and territories responsible for strategizing vaccine roll-outs could refine the prioritizations based on their own regional demographics.
|
What this means for inflammatory arthritis patients A question top-of-mind for inflammatory arthritis patients is whether the COVID-19 vaccine’s effectiveness could be affected by immunosuppressant medications, such as disease-modifying antirheumatic drugs (DMARDs) and biologics. When it comes to any new vaccine, people living with autoimmune diseases — such as rheumatoid arthritis, axial spondyloarthritis, lupus, inflammatory bowel disease, psoriasis or multiple sclerosis — have long had vaccine worries that the general public doesn’t. There are two general main concerns:
As of December 2020, NACI recommends that the COVID-19 vaccine “should not be offered to patients who are immunosuppressed due to disease or treatment or those with an autoimmune disorder until further evidence is available. However, a complete series of COVID-19 vaccine may be offered to individuals in the authorized age group in this population if a risk assessment deems that the benefits outweigh the potential risks for the individual, and if informed consent includes discussion about the absence of evidence on the use of COVID-19 vaccine in this population.”2 Based on the absence of safety or efficacy data in patients living with active autoimmune disease, such as inflammatory arthritis, some provinces and territories are not currently planning to administer the vaccine to people who are immunocompromised. ACE is monitoring this issue closely and will continue to provide updates as policies evolve on who should receive the COVID-19 vaccine. |

But after essential groups, who comes next?
Canada’s chief public health officer Dr. Theresa Tam said that according to what the science suggests about who is most at risk from COVID-19, the initial round of vaccines should go to those in high-risk situations such as hospitals and care homes. The next batch, she added, should be done by age, with the oldest at the front of the line: “We know that underlying medical conditions put people at high risk but when we actually analyze all the different underlying medical conditions, and their age, it still comes out that the age is in fact the most important where you look at severe illness and mortality.”3
Some provinces, like Alberta, have floated the idea, the vaccines should be distributed by population. Governments will also be listening carefully to the pleas from employers whose businesses have been severely disrupted due to COVID-19 to ensure their employees are prioritized to get vaccinated. A recent Statistics Canada survey from mid-September to late October found that five per cent of businesses were actively considering bankruptcy or closure this fall. Anxieties are running highest among the arts, entertainment and hospitality industries, with nearly 30 per cent worried they’ll need to resort to layoffs, bankruptcy or closure within six months.
There are other important ethical and societal consideration on who should be prioritized and is related to how disproportionately COVID-19 has affected ethnic and low-income Canadians. As ACE has reported throughout the pandemic, researchers have found Black, South Asian and Indigenous Canadians are far more likely than white Canadians to have multiple medical conditions putting them at higher risk of severe outcomes, including mortality, from COVID-19.
In our Fall issue of JointHealth™ insight, we also looked at the significantly higher percentage of COVID-19 cases happening in visible minorities as well as low-income households.
According to Prime Minister Trudeau reporting after a first minister’s call on November 12, 2020, there seems to be a consensus among federal, provincial and territory government that we should all agree across the country on what the prioritization list looks like and make sure that it is applied fairly right across the country.4
Given the health inequities that historically exist in Canada (see ACE’s Arthritis Medications Report Card), whatever happens when Canadians line up to be vaccinated, we can anticipate there will potentially be a period of time in 2021 when the limited supply of vaccines will create a society of haves and have-nots.

Immunity passports?
The idea of “immunity passports” was floated early on in the pandemic as some governments expressed optimism that individuals who’d recovered from COVID-19 and tested positive for virus-fighting antibodies could be given greater freedoms to travel or return to work. However, the World Health Organization dismissed the idea, saying there wasn’t enough evidence yet on the effectiveness or longevity of immunity through antibodies.
Vaccines may give new attention to the notion of “immunity passports” -- a possibility that public health experts say needs to be handled thoughtfully. For example, these experts describe scenarios where employers and regulators use people’s immune status to selectively grant them access to employment and travel.
What happens if you suffer side effects?
As Canada gets closer to authorizing more COVID-19 vaccines, many ACE members have been asking what it will feel like to get it? Is it going to be like the flu vaccine? Will it be more painful? And what about side-effects?
The two front-runners for getting an emergency use authorization from Health Canada - Pfizer and Moderna -- use new mRNA technology. These vaccines require two doses: one to prime the body, and then a few weeks later, a second shot to boost the response. Study results show that Pfizer and Moderna’s vaccines are each in the range of 95% effective. But because the technology is so new for a vaccine, it has raised many questions and some public concerns.
All COVID-19 vaccines currently being studied are tested for both their effectiveness and safety. Before reaching the general public, Health Canada needs to authorize that the vaccine is safe enough for public use. Even so, there’s a chance that some individuals could suffer long-term side effects from a COVID-19 vaccine.
In the rare event that someone suffers negative side effects of the vaccine, some public health experts believe they should be financially compensated. More than 20 countries, including all other G7 countries, have programs that compensate individuals injured by vaccines. The Government of Canada announced on December 10, 2020 that it will be introducing an injury support program for all vaccines approved by Health Canada, including those developed for COVID-19. As stated by the Public Health Agency of Canada: ,“ building on the model in place in Québec for over 30 years, the program will ensure that all Canadians have to have fair access to support in the rare event that they experience an adverse reaction to a vaccine”.

Can you choose which vaccine you want?
With seven vaccine candidates in the race to be authorized after Pfizer’s, Canada will have several different vaccines on the market in 2021. However, experts say that there is no health benefit to receiving more than one type of vaccine. As for personal choice, it’s unlikely that Canadians will have the option to choose which vaccine they want. Instead, it will depend upon the agreement the provinces and territories reach with the federal government on how many doses of a particular vaccine they receive. The primary issue for these jurisdictions as the vaccines arrive in Canada will not be choice but prioritizing the population segments to receive the vaccine.
 Can you refuse the vaccine?
Can you refuse the vaccine?Over the course of the pandemic since the outbreak in March 2020, vaccine confidence has declined and a consistent portion of Canadians remain undecided about whether to get vaccinated.
According to Government of Canada surveys, 65% of respondents strongly agree or agree that they would get a safe vaccine if it becomes available and only 43% think that vaccines are completely safe. Twenty-four per cent of Canadians are neutral or undecided about whether to get vaccinated. Concerns around a lack of research and testing, the safety/effectiveness of a vaccine, and the newness of the vaccine were the most prevalent reasons for not wanting to receive a safe vaccine once developed.5
It’s impossible for anyone to be forced to take the COVID-19 vaccine once it’s available. But there could be real-life consequences to refusal. For instance, individuals who aren’t vaccinated may miss out on returning to the workplace or could face other restrictions involving group gatherings.
 The distrust people have in the COVID-19 vaccine is part of a long-standing anti-vaccination movement in North America, but also a product of the “infodemic” that has coincided with the pandemic. In an August JointHealth™ insight, ACE focused on this infodemic as defined by the World Health Organization as “an overabundance of information, some accurate and some not—that makes it hard for people to find trustworthy sources and reliable guidance when they need it.”
The distrust people have in the COVID-19 vaccine is part of a long-standing anti-vaccination movement in North America, but also a product of the “infodemic” that has coincided with the pandemic. In an August JointHealth™ insight, ACE focused on this infodemic as defined by the World Health Organization as “an overabundance of information, some accurate and some not—that makes it hard for people to find trustworthy sources and reliable guidance when they need it.”Even when people have access to high-quality information on the vaccine, misinformation about it continues to spread further and faster and adds complexity to our trust and acceptance of its safety and efficacy. We have seen a similar phenomenon over the past year with the decision to not wear a mask as a means to slow the spread of the virus, which has had less to do with the pandemic than a distrust in authorities and science.
Governments, healthcare leaders and the digital platforms where people find the misinformation must address the “fake news” that undermines our shared ability to vaccinate against COVID-19 and build trust in the communities where vaccine misinformation has taken root.
An example of that effort occurred on December 3, 2020, when Facebook announced it would remove posts that contain claims about COVID-19 vaccines that have been discredited or contradicted by health groups including the World Health Organization, the United States Food and Drug Administration and the Centers for Disease Control and Prevention.6
The World Health Organization has prepared a guide – “How to respond to a vaccine denier” - to help organizations and individuals respond to vaccination misinformation. Click here to learn more.
How to make this holiday fun, safe and healthy
Home for the holidays takes on a new meaning this year. Here are some tips to help you have a happy holiday during the pandemic.
Make holiday shopping safe and simple
- Consider buying gifts online; it is less stressful, convenient, protects you from possible exposure to COVID-19 in shopping malls and saves energy.
- Consider using curb side pick-up or delivery services for your online purchases.
- Shop local to support small businesses and avoid expensive shipping and handling fees.
Keep those joints moving!
Research has shown that physical activity is an important way for people living with arthritis to manage joint pain and increase mobility. Below are some tips on staying motivated and exercising over the holiday break:- Opt to do an exercise program you enjoy – it will be much easier to stick to the program if you like what you are doing.
- Find an exercise buddy – in-person with a housemate or virtually with friends.
- Consider following along with Dr. Jasmin Ma’s 15-minute exercise “snacks” from our Arthritis at Home program. She runs 4 different up-beat exercise sessions for people living with arthritis.
- Try this arthritis-friendly mini yoga class with yoga therapist Lindsay Knazan. She demonstrates different tools and poses that people with arthritis can practice from their homes using a tennis ball, a wall, and a chair.
Make a list and check it twice
The holidays can be a busy, stressful time. Your mental health is important. Make planning easier. Write out a list of all the tasks that need to be accomplished during the holidays, and:- Consider making a schedule and ask for help – ask a neighbour to shovel snow for you or ask a family member to do a particular errand for you.
- Categorize your list from highest to lowest priority.
- Plan activities according to how you feel and be flexible with your schedule.
- Consider skipping the ones of lowest priority.

Make informed decisions about participating in different holiday activities
Depending on where you live in Canada, you may have to make some difficult decisions this holiday season about who you will interact with and how you will interact with them. ACE broke down decision making into 3 key steps, briefly summarized below. *Read the September issue of JointHealth™ insight for more tips on health and wellness decision making during COVID-19:- Ensure the activity does not go against public health policies in your area
- Determine risk level of the activity: The risk level of an activity will generally depend on the number of COVID-19 cases in your community and the specific setting in which the activity takes place. In general, risk increases with the amount of time spent in closed spaces with poor ventilation, the number of people present, and the likelihood of “forceful exhalation” such as sneezing, coughing or yelling.
- Consider the unique circumstances of yourself and your loved ones. Ask yourself questions like: How will participating in this activity impact me or those I care about? How important is this activity to me? Will I have the chance to do this another time in the future? Do I feel that I have enough information and support to make this decision?
Entertainment at Home
- If you get tired of social gatherings on Zoom, playing games online or scrolling through social media, here is daily list of interesting films and TV shows to stream over the holidays.
- You may also want to check our Arthritis At Home video interviews and podcasts with Canadians experts in clinical rheumatology, researchers, allied health professionals and patient experts.

Stay Connected
The pandemic is a time to stay connected. Social interaction is vital for both mental and physical health. A new national survey by the Canadian Mental Health Association and the University of British Columbia found that 40 per cent of people surveyed said that their mental health had deteriorated since the COVID-19 outbreak began – a figure that rose to 61 per cent among those with a pre-existing mental-health issue. With restrictions to in-person interactions, we are forced to find creative ways to make the holidays special:- Have a video or telephone call with a friend or family member while you cook the same festive meal.
- Arrange a virtual meet up with friends or families.
- Go outside for some fresh air – enjoy a socially distanced walk while following local health orders.
- Participate in online interest classes or events.
- Get creative! Think of modified versions of your favourite holiday traditions with others, such as a contactless cookie exchange.
- Dr. Susan Bartlett talks about how we can reconnect with loved ones during COVID-19 and take this opportunity to meet new people in this Arthritis at Home episode.
- Get in touch with your healthcare team if you have concerns about your physical or mental health.
| 1 | National Post, “COVID-19 vaccine: A look at how provinces and territories are readying for rollout,” November 30, 2020. https://nationalpost.com/news/a-look-at-what-provinces-and-territorieshave-said-about-covid-19-vaccine-plans-4 |
| 2 | Public Health Agency of Canada: National Advisory Committee on Immunization recommendations on the use of COVID-19 vaccine(s) – December 12, 2020 - https://www.canada.ca/en/public-health/services/immunization/national-advisory-committee-on-immunization-naci/recommendations-use-covid-19-vaccines.html |
| 3 | Canada News Media, “PM: Feds, provinces agree vaccine prioritization should be consistent Canada-wide”, December 1, 2020 - https://canadanewsmedia.ca/pm-feds-provinces-agree-vaccineprioritization-should-be-consistent-canada-wide-ctv-news/ |
| 4 | Canada News Media, “PM: Feds, provinces agree vaccine prioritization should be consistent Canada-wide”,December 1, 2020 - https://canadanewsmedia.ca/pm-feds-provinces-agree-vaccineprioritization-should-be-consistent-canada-wide-ctv-news/ |
| 5 | Impact Canada, “COVID-19 Snapshot Monitoring – Wave 8 Results” https://impact.canada.ca/en/challenges/cosmo-canada/wave8 |
| 6 | Consumer Reports, “Facebook Will Remove COVID-19 Vaccine Misinformation,” December 3, 2020 https://www.consumerreports.org/social-media/facebook-will-remove-covid-19-vaccinemisinformation/ |
Listening to you
We hope you find this information of use. Please tell us what you think by writing to us or emailing us at feedback@jointhealth.org. Through your ongoing and active participation, ACE can make its work more relevant to all Canadians living with arthritis.
Update your email or postal address
Please let us know of any changes by contacting ACE at feedback@jointhealth.org. This will ensure that you continue to receive your free email or print copy of JointHealth™ insight.
Arthritis Consumer Experts (ACE)
Who We Are
Arthritis Consumer Experts (ACE) operates as a non-profit and provides free research based education and information to Canadians with arthritis. We help (em)power people living with all forms of arthritis to take control of their disease and to take action in healthcare and research decision making. ACE activities are guided by its members and led by people with arthritis, scientific and medical experts on the ACE Advisory Board. To learn more about ACE, visit www.jointhealth.org
Disclosures
Over the past 12 months, ACE received grants- in-aid from: Arthritis Research Canada, Amgen Canada, Canadian Institutes of Health Research, Canadian Rheumatology Association, Eli Lilly Canada, Hoffman-La Roche Canada Ltd., Knowledge Translation Canada, Merck Canada, Novartis Canada, Pfizer Canada, Sandoz Canada, Sanofi Canada, St. Paul’s Hospital (Vancouver), UCB Canada, and the University of British Columbia.
ACE also received unsolicited donations from its community members (people with arthritis) across Canada.
ACE thanks funders for their support to help the nearly 6 million Canadians living with osteoarthritis, rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis and the many other forms of the disease.
Disclaimer
The material contained on this website is provided for general information only. This website should not be relied on to suggest a course of treatment for a particular individual or as a substitute for consultation with qualified health professionals who are familiar with your individual medical needs. Should you have any healthcare related questions, you should contact your physician. You should never disregard medical advice or delay in seeking it because of something you have read on this or any website.
This site may provide links to other Internet sites only for the convenience of World Wide Web users. ACE is not responsible for the availability or content of these external sites, nor does ACE endorse, warrant or guarantee the products, services or information described or offered at these other Internet sites.
Although the information presented on this website is believed to be accurate at the time it is posted, this website could include inaccuracies, typographical errors or out-of-date information. This website may be changed at any time without prior notice.
