In this issue
- JointHealth™ Education: Psoriatic Arthritis and Ankylosing Spondylitis
- ACE launches new JointHealth™ Education Psoriatic Arthritis and Ankylosing Spondylitis courses
- What is JointHealth™ Education?
- JHED: PsA, AS: What you'll learn
- JHED PsA: Psychosocial experiences and unmet treatment expectations of patients with PsA and psoriasis
- JHED AS: Exercise recommendations in ankylosing spondylitis
- Are you a JointHealth™ Education graduate?
JointHealth™ insight Published July 2019

Arthritis Consumer Experts (ACE) has launched two new JointHealth™ Education courses: JHEd PsA and JHEd AS. Each disease specific course includes 6 lessons that are interactive and evidence-based. The courses are designed to empower PsA and AS patients by equipping them with the knowledge, skills and confidence to be equal partners on their healthcare team.
Each course gives you the key facts or “speaking points” to cover during your appointments with your rheumatologist and in your life with family, friends and at work. The Lesson Plan starts with information and tips on fine tuning your communication and listening skills and ends with information on how to manage your world with PsA or AS in between your appointments. Each lesson includes easy to read content, a short quiz and a coaching video for your viewing. When all three lessons are completed, you will receive a “graduation certificate” by email.
The courses highlight different disease specific information based on the latest research and clinical recommendations. The psoriatic arthritis course is also based on findings from a recent global study on the experiences of people living with PsA. The content for each course has been reviewed by a board of scientific directors and rheumatologists to ensure clinical accuracy.
 What you'll learn
What you'll learn

Psychosocial experiences and unmet treatment expectations of patients with PsA and psoriasis
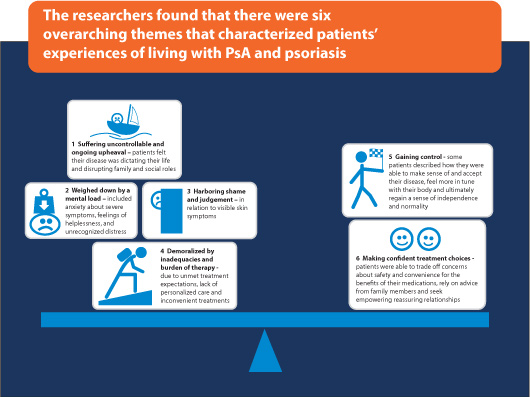
In March 2019, Dr. Danial Sumpton, Rheumatologist, Concord Repatriation General Hospital, and his research team published a study1 that aimed to identify gaps in patient care for PsA and psoriasis. The team conducted a systematic literature review, analyzing a large number of existing studies from around the world that looked at experiences of adult patients with PsA and psoriasis. The review allowed researchers to look at more data on patient experience then could be collected with one individual study. Sumpton and his team analysed 56 studies that represented 1,147 patients with psoriasis and 337 patients with PsA. These studies collected information about patient experiences through individual interviews as well as focus groups where several patients shared their experiences together in the same room.
These findings are both concerning and encouraging. While they point to significant gaps in care for psychosocial symptoms of PsA and psoriasis, uncovering these gaps is the first step towards addressing them. In addition, the study shows that there are also ways to feel empowered and in control of one’s disease. Sumpton added: “[patients] felt empowered when they developed an understanding of the pathophysiology [i.e. disease] and link between psoriasis and arthritis and gained a broader insight into treatment options to advocate for their use.” Arthritis Consumer Experts’ online education course can help patients do exactly this. JHEd PsA helps patients build disease knowledge and communication skills so that they can be equal partners on their healthcare team. This ensures that the patients’ values and goals are accounted for and that they feel confident about their treatment plan rather than feeling disempowered by unmet treatment expectations. The course also provides tips on how to care for your mental health, feel in control of your disease, and manage social and intimate relationships. To learn more about the complex relationship between mental health and arthritis, read our February 2019 issue of JointHealth™ insight.
1 Sumpton D, et al. “Patients’ perspectives and experience of psoriasis and psoriatic arthritis: a systematic review and thematic synthesis of qualitative studies”. Arthritis Care and Research. March 2019 https://doi.org/10.1002/acr.23896.

Exercise recommendations in ankylosing spondylitis
There is an international consensus that exercise is beneficial in ankylosing spondylitis (AS), but there is little information to guide the type and amount of exercise needed for most benefit. Recently, a team of Australian researchers released 10 evidence-based and consensus-based exercise recommendations, which were published in Science Direct and featured in RheumNow.2 “This collaborative project, combining evidence with clinical expertise, was established to develop practical recommendations to guide sustainable exercise prescription for individuals with AS,” said lead author Janet Milner, Physiotherapist, Menzies Institute for Medical Research, University of Tasmania.
2 Milner J, et al. “Exercise for ankylosing spondylitis: An evidence-based consensus statement” Science Direct. February 2016. https://doi.org/10.1016/j.semarthrit.2015.08.003.
Listening to you
We hope you find this information of use. Please tell us what you think by writing to us or emailing us at feedback@jointhealth.org. Through your ongoing and active participation, ACE can make its work more relevant to all Canadians living with arthritis.
Update your email or postal address
Please let us know of any changes by contacting ACE at feedback@jointhealth.org. This will ensure that you continue to receive your free email or print copy of JointHealth™ insight.
Arthritis Consumer Experts (ACE)
Who We Are
Arthritis Consumer Experts (ACE) operates as a non-profit and provides free research based education and information to Canadians with arthritis. We help (em)power people living with all forms of arthritis to take control of their disease and to take action in healthcare and research decision making. ACE activities are guided by its members and led by people with arthritis, scientific and medical experts on the ACE Advisory Board. To learn more about ACE, visit www.jointhealth.org
Disclosures
Over the past 12 months, ACE received grants-in-aid from: Amgen, Arthritis Research Canada, Canadian Biosimilars Forum, Canadian Institutes of Health Research, Canadian Rheumatology Association, Eli Lilly Canada, Hoffman-La Roche Canada Ltd., Knowledge Translation Canada, Merck Canada, Novartis Canada, Pfizer Canada, Sandoz Canada, Sanofi Canada, UCB Canada, and the University of British Columbia.
ACE also received unsolicited donations from its community members (people with arthritis) across Canada.
ACE thanks funders for their support to help the nearly 6 million Canadians living with osteoarthritis, rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis and the many other forms of the disease.
Disclaimer
The material contained on this website is provided for general information only. This website should not be relied on to suggest a course of treatment for a particular individual or as a substitute for consultation with qualified health professionals who are familiar with your individual medical needs. Should you have any healthcare related questions, you should contact your physician. You should never disregard medical advice or delay in seeking it because of something you have read on this or any website.
This site may provide links to other Internet sites only for the convenience of World Wide Web users. ACE is not responsible for the availability or content of these external sites, nor does ACE endorse, warrant or guarantee the products, services or information described or offered at these other Internet sites.
Although the information presented on this website is believed to be accurate at the time it is posted, this website could include inaccuracies, typographical errors or out-of-date information. This website may be changed at any time without prior notice.

|
ACE launches new JointHealth™ Education Psoriatic Arthritis and Ankylosing Spondylitis courses In this issue of JointHealth™ insight, we introduce two new JointHealth™ Education (JHEd) courses: Psoriatic Arthritis (PsA) and Ankylosing Spondylitis (AS). We take an in-depth look at the courses and share new research findings in both disease areas, including psychosocial experiences of patients with PsA and new exercise recommendations for AS. |
“JointHealth™ Education was inspired by many of ACE’s members living with an inflammatory arthritis who have told us they lack the knowledge and communications skills to have full, satisfying conversations with their rheumatologists. A patient’s perception of their inflammatory arthritis, such as PsA or AS and its treatment, as well as their relationship with their healthcare provider, impacts the management and the outcomes of their disease.
Our graduates who have taken JointHealth™ Education courses have told us
 the program has improved their ability to communicate with their rheumatologists and helped achieve the best possible outcomes for their disease management.”
the program has improved their ability to communicate with their rheumatologists and helped achieve the best possible outcomes for their disease management.”Cheryl Koehn, Founder and President, Arthritis Consumer Experts. “Canadian rheumatologists have been actively discussing and pursuing ways to improve communication between patients and rheumatologists in order to work together to set treatment goals and establish a treatment plan to achieve the best possible disease outcomes. JointHealth™ Education is a great program not just for patients, but also for rheumatologists – junior and senior, alike. We need to see our patient’s experiences,  needs and goals through their eyes and words.”
needs and goals through their eyes and words.”Kam Shojania, MD, FRCPC, Clinical Professor and Head, Division of Rheumatology, University of British Columbia, and Medical Director of the Mary Pack Arthritis Program. |
Each course gives you the key facts or “speaking points” to cover during your appointments with your rheumatologist and in your life with family, friends and at work. The Lesson Plan starts with information and tips on fine tuning your communication and listening skills and ends with information on how to manage your world with PsA or AS in between your appointments. Each lesson includes easy to read content, a short quiz and a coaching video for your viewing. When all three lessons are completed, you will receive a “graduation certificate” by email.
The courses highlight different disease specific information based on the latest research and clinical recommendations. The psoriatic arthritis course is also based on findings from a recent global study on the experiences of people living with PsA. The content for each course has been reviewed by a board of scientific directors and rheumatologists to ensure clinical accuracy.
|
What is JointHealth™ Education? The JointHealth™ Education program was launched in 2016 and now includes five user friendly, on-line, courses:
|
 What you'll learn
What you'll learnLesson 1
The Art of Communication with Your Rheumatologist
Topics include:
The Art of Communication with Your Rheumatologist
- Getting ready for your appointment with your rheumatologist
- Getting comfortable in your rheumatologist’s office
- Communication warm-up
- The essentials for effective communication with your rheumatologist
Lesson 2
Understanding your PsA or AS diagnosis
Topics include:
Understanding your PsA or AS diagnosis
- The facts about PsA or AS
- Getting diagnosed
- Treatment basics
- The latest research on PsA or AS
Lesson 3
Setting treatment goals and building a treatment plan
Topics include:
Setting treatment goals and building a treatment plan
- Time management
- Asking questions, sharing fears and concerns, and listening
- Setting treatment goals
- Making a treatment plan
Lesson 4
Talking about PsA or AS treatments
Topics include:
Talking about PsA or AS treatments
- Evidence-based treatments
- Making treatment choices with your rheumatologist
- Sticking with your treatments
- Monitoring the effectiveness of your treatments and treatment plan
Lesson 5
Self-care and PsA or AS
Topics include:
Self-care and PsA or AS
- Taking charge of what you can control
- Elements of a self-care plan
- At-home self-care treatments
- Caring for your mental health
- Sharing your self-care success with your rheumatologist
Lesson 6
Managing your world with PsA or AS
Topics include:
Managing your world with PsA or AS
- How to explain PsA or AS to the people in your world
- PsA or AS and its effect on relationships
- Communication tips to help you in your disease journey
- Asking for support and help
- Your sexuality and PsA or AS
- Your disease at work

Psychosocial experiences and unmet treatment expectations of patients with PsA and psoriasis
In March 2019, Dr. Danial Sumpton, Rheumatologist, Concord Repatriation General Hospital, and his research team published a study1 that aimed to identify gaps in patient care for PsA and psoriasis. The team conducted a systematic literature review, analyzing a large number of existing studies from around the world that looked at experiences of adult patients with PsA and psoriasis. The review allowed researchers to look at more data on patient experience then could be collected with one individual study. Sumpton and his team analysed 56 studies that represented 1,147 patients with psoriasis and 337 patients with PsA. These studies collected information about patient experiences through individual interviews as well as focus groups where several patients shared their experiences together in the same room.
These findings are both concerning and encouraging. While they point to significant gaps in care for psychosocial symptoms of PsA and psoriasis, uncovering these gaps is the first step towards addressing them. In addition, the study shows that there are also ways to feel empowered and in control of one’s disease. Sumpton added: “[patients] felt empowered when they developed an understanding of the pathophysiology [i.e. disease] and link between psoriasis and arthritis and gained a broader insight into treatment options to advocate for their use.” Arthritis Consumer Experts’ online education course can help patients do exactly this. JHEd PsA helps patients build disease knowledge and communication skills so that they can be equal partners on their healthcare team. This ensures that the patients’ values and goals are accounted for and that they feel confident about their treatment plan rather than feeling disempowered by unmet treatment expectations. The course also provides tips on how to care for your mental health, feel in control of your disease, and manage social and intimate relationships. To learn more about the complex relationship between mental health and arthritis, read our February 2019 issue of JointHealth™ insight.
1 Sumpton D, et al. “Patients’ perspectives and experience of psoriasis and psoriatic arthritis: a systematic review and thematic synthesis of qualitative studies”. Arthritis Care and Research. March 2019 https://doi.org/10.1002/acr.23896.

Exercise recommendations in ankylosing spondylitis
There is an international consensus that exercise is beneficial in ankylosing spondylitis (AS), but there is little information to guide the type and amount of exercise needed for most benefit. Recently, a team of Australian researchers released 10 evidence-based and consensus-based exercise recommendations, which were published in Science Direct and featured in RheumNow.2 “This collaborative project, combining evidence with clinical expertise, was established to develop practical recommendations to guide sustainable exercise prescription for individuals with AS,” said lead author Janet Milner, Physiotherapist, Menzies Institute for Medical Research, University of Tasmania.
|
2 Milner J, et al. “Exercise for ankylosing spondylitis: An evidence-based consensus statement” Science Direct. February 2016. https://doi.org/10.1016/j.semarthrit.2015.08.003.
|
Are you a JointHealth™ Education graduate? Have you completed one of ACE’s JointHealth™ Education courses? How has it helped you discuss what is most important for you in terms of treatment success? Are you more comfortable raising concerns/fear with your rheumatologist and asking questions during your clinical visit? Your responses will help us improve our program and ensure it delivers what patients want. Please email your comments to feedback@jointhealth.org. |
Listening to you
We hope you find this information of use. Please tell us what you think by writing to us or emailing us at feedback@jointhealth.org. Through your ongoing and active participation, ACE can make its work more relevant to all Canadians living with arthritis.
Update your email or postal address
Please let us know of any changes by contacting ACE at feedback@jointhealth.org. This will ensure that you continue to receive your free email or print copy of JointHealth™ insight.
Arthritis Consumer Experts (ACE)
Who We Are
Arthritis Consumer Experts (ACE) operates as a non-profit and provides free research based education and information to Canadians with arthritis. We help (em)power people living with all forms of arthritis to take control of their disease and to take action in healthcare and research decision making. ACE activities are guided by its members and led by people with arthritis, scientific and medical experts on the ACE Advisory Board. To learn more about ACE, visit www.jointhealth.org
Disclosures
Over the past 12 months, ACE received grants-in-aid from: Amgen, Arthritis Research Canada, Canadian Biosimilars Forum, Canadian Institutes of Health Research, Canadian Rheumatology Association, Eli Lilly Canada, Hoffman-La Roche Canada Ltd., Knowledge Translation Canada, Merck Canada, Novartis Canada, Pfizer Canada, Sandoz Canada, Sanofi Canada, UCB Canada, and the University of British Columbia.
ACE also received unsolicited donations from its community members (people with arthritis) across Canada.
ACE thanks funders for their support to help the nearly 6 million Canadians living with osteoarthritis, rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis and the many other forms of the disease.
Disclaimer
The material contained on this website is provided for general information only. This website should not be relied on to suggest a course of treatment for a particular individual or as a substitute for consultation with qualified health professionals who are familiar with your individual medical needs. Should you have any healthcare related questions, you should contact your physician. You should never disregard medical advice or delay in seeking it because of something you have read on this or any website.
This site may provide links to other Internet sites only for the convenience of World Wide Web users. ACE is not responsible for the availability or content of these external sites, nor does ACE endorse, warrant or guarantee the products, services or information described or offered at these other Internet sites.
Although the information presented on this website is believed to be accurate at the time it is posted, this website could include inaccuracies, typographical errors or out-of-date information. This website may be changed at any time without prior notice.
